PRP Therapy for Knee Pain 101: Review 2023
Osteoarthritis (OA) is the most common type of arthritis. OA of the knee happens when the cartilage — the cushion between the knee joints — breaks down. This can cause pain, stiffness, and swelling.
There is no cure for OA of the knee, but treatment can help relieve discomfort and slow the damage. It can improve also your quality of life and help you better keep up with your day-to-day activities.
Your treatment options will depend on your individual needs. These include your medical history, level of pain, and the impact of OA on your daily life.
Treatment usually includes a combination of therapies and lifestyle choices.
There is no cure for OA of the knee, but treatment can help relieve discomfort and slow the damage. It can improve also your quality of life and help you better keep up with your day-to-day activities.
Your treatment options will depend on your individual needs. These include your medical history, level of pain, and the impact of OA on your daily life.
Treatment usually includes a combination of therapies and lifestyle choices.
Platelet-rich plasma (PRP) is a novel treatment for managing pain related to osteoarthritis (OA) of the knee. Some PRP preparations have approval from the US Food and Drug Administration (FDA), but approval does not yet cover the use of PRP in OA of the knee. Nevertheless, some clinics may offer it “off-label”.
There is nothing in medicine that gets away from the concept of dose. Meaning, if you give the patient the right dose, they get better. If you give the wrong dose, there is no effect. PRP is NO EXCEPTION.
We have tested the concept that the dose of PRP needed is age-dependent numerous times. Meaning younger patients can get by with lower doses. Older patients need much higher doses. How do I know this?
Take our recent published study on tenocytes (tendon cells). When we exposed young tenocytes to PRP they maxed out their ability to heal at low concentrations. However, when old tenocytes were exposed to PRP, the ability to heal was stimulated by a direct dose-response relationship. In other words, the higher the PRP concentration, the more lab-based evidence of healing we observed.
Hence, if you’re young (under the age of 35), you probably don’t need to worry about the PRP dose. However, if you’re middle-aged or older, this is a VERY BIG DEAL that can make the difference between a failed and successful treatment. How high should that dose be?
Based on our published research, if you’re older, this is what we recommend:
Where the PRP is placed is CRITICAL. Meaning if you want to promote healing in a specific structure, you MUST get the PRP accurately inside that structure.
There are a number of categories here:
Insurance companies consider PRP an experimental treatment. More scientific research will have to conclude its effectiveness before it is more widely covered.
Some PRP treatments for knee are also done in combination with add on hyaluronic acid injection.
We hope you’ve gained the ability now to separate the poor quality clinics that are not a good value from the high-quality clinics that can deliver a much better product.
Being a consumer of high-quality healthcare these days takes lots of homework. We hope this guide to high-quality PRP injections helps you find a clinic that has all of the tools needed to help you recover!
Knee gel injections cost
Following is a review of the available effectiveness data taken from clinical, and real-world studies of PRP in knee Osteoarthritis.


There are literally more PRP kits for sale nowadays. Each produces a completely different PRP product. Some of these kits produce junk PRP and some produce high-quality PRP. How would you know?
The other way PRP is processed is through an onsite lab. This could be a very bad or good thing. For example, on the bad side, an improperly run and supervised on-site lab may introduce bacterial contamination or make a bad PRP product. Having said that, a properly supervised and run lab can produce better quality PRP products in more variety than any PRP kit on the market.
The workhorse of modern PRP use is the amber LP-PRP. Why? While the research bounces back and forth on this one, right now, we have more evidence that amber LP-PRP is more effective for common everyday uses like knee arthritis and tendon problems. However, every rule in medicine has an exception. For the injection of spinal discs (and NOT other areas in the spine), high-dose LR-PRP, based on recent research is likely safer because it helps fight the bacteria that could cause a nasty side effect called discitis.
So unless you’re getting your disc injected, you want the PRP to be amber in color.


PRP Studies for Knee Arthritis
One study assessing PRP’s efficacy was a meta-analysis recently published in Sports Health: A Multidisciplinary Approach. For this systematic review, researchers queried MEDLINE, EMBASE, Cochrane, CINAHL, SPORTDiscus, and Web of Science libraries through Feb. 8, 2017, and collected data from reviews, trials registries, and recent conferences. Studies eligible for inclusion were randomized trials published in English that compared platelet-rich therapy to a control, assessing patients aged ≥ 18 years with musculoskeletal bone, cartilage, or soft tissue injuries.
The final analysis included 78 randomized controlled trials with a total of 5,308 patients. The researchers considered a standardized mean difference (SMD) of 0.5 as the minimum for significant pain reduction. At three months, PRP was associated with reduced pain (SMD, –0.34; 95% CI, –0.48 to –0.20), which was also observed at one year (SMD, –0.60; 95% CI, –0.81 to –0.39). In lateral epicondylitis, evidence supporting PRP use was low- to moderate-quality (SMD, –0.69; 95% CI, –1.15 to –0.23) at one year; low- to moderate-quality one-year evidence also supported PRP use in knee OA (SMD, –0.91; 95% CI, –1.41 to –0.41).
Another study, published in the Journal of Back and Musculoskeletal Rehabilitation, evaluated PRP specifically in patients with knee OA. A total of 60 patients with chronic knee pain were randomized to receive 4 mL PRP intra-articularly (IA) in three doses once a week or one 4 mL dose of saline solution IA. Pain and functional outcomes were assessed using the Visual Analog Scale (VAS) and Western Ontario and McMaster University Osteoarthritis Index (WOMAC), respectively, and ultrasonography (USG) was used to determine distal femur cartilage thickness.
After one month, the PRP group had significantly reduced VAS scores (P < 0.001) and WOMAC pain sub-scores. At six months, VAS scores remained low in the PRP group, and all WOMAC parameters were significantly lower compared to the placebo group. Cartilage thickness did not differ between the groups.
A third study, published in the Journal of Orthopaedic Research, evaluated whether cartilage thickness played a role in outcomes for knee OA patients undergoing PRP therapy. This trial included 59 patients who underwent PRP with a low-leukocyte autologous conditioned plasma (ACP) system. Patients underwent MRI prior to treatment; researchers collected patients’ Whole-Organ MRI Score (WORMS), which determined knee OA level based on 14 parameters: integrity of the cartilage, affection of the bone marrow, subcortical cysts, bone attrition, osteophytes, integrity of the menisci and ligaments, presence of synovitis, loose bodies, and periarticular cysts.
Per the WORMS Cartilage Score, OA severity was classified as mild (20.3%), moderate (55.9%), and severe (23.7%). After PRP therapy, VAS scores decreased by 3.58 points, and WOMAC-Score decreased by 23.51 points. There were no significant differences in pain improvement based on OA level; the researchers concluded, “The findings of the current study suggest that positive effects of intra-articular injections of PRP might improve quality of life and reduce the pain of patients suffering from osteoarthritis of the knee joint independent from the level of cartilage damage.”
The final analysis included 78 randomized controlled trials with a total of 5,308 patients. The researchers considered a standardized mean difference (SMD) of 0.5 as the minimum for significant pain reduction. At three months, PRP was associated with reduced pain (SMD, –0.34; 95% CI, –0.48 to –0.20), which was also observed at one year (SMD, –0.60; 95% CI, –0.81 to –0.39). In lateral epicondylitis, evidence supporting PRP use was low- to moderate-quality (SMD, –0.69; 95% CI, –1.15 to –0.23) at one year; low- to moderate-quality one-year evidence also supported PRP use in knee OA (SMD, –0.91; 95% CI, –1.41 to –0.41).
Another study, published in the Journal of Back and Musculoskeletal Rehabilitation, evaluated PRP specifically in patients with knee OA. A total of 60 patients with chronic knee pain were randomized to receive 4 mL PRP intra-articularly (IA) in three doses once a week or one 4 mL dose of saline solution IA. Pain and functional outcomes were assessed using the Visual Analog Scale (VAS) and Western Ontario and McMaster University Osteoarthritis Index (WOMAC), respectively, and ultrasonography (USG) was used to determine distal femur cartilage thickness.
After one month, the PRP group had significantly reduced VAS scores (P < 0.001) and WOMAC pain sub-scores. At six months, VAS scores remained low in the PRP group, and all WOMAC parameters were significantly lower compared to the placebo group. Cartilage thickness did not differ between the groups.
A third study, published in the Journal of Orthopaedic Research, evaluated whether cartilage thickness played a role in outcomes for knee OA patients undergoing PRP therapy. This trial included 59 patients who underwent PRP with a low-leukocyte autologous conditioned plasma (ACP) system. Patients underwent MRI prior to treatment; researchers collected patients’ Whole-Organ MRI Score (WORMS), which determined knee OA level based on 14 parameters: integrity of the cartilage, affection of the bone marrow, subcortical cysts, bone attrition, osteophytes, integrity of the menisci and ligaments, presence of synovitis, loose bodies, and periarticular cysts.
Per the WORMS Cartilage Score, OA severity was classified as mild (20.3%), moderate (55.9%), and severe (23.7%). After PRP therapy, VAS scores decreased by 3.58 points, and WOMAC-Score decreased by 23.51 points. There were no significant differences in pain improvement based on OA level; the researchers concluded, “The findings of the current study suggest that positive effects of intra-articular injections of PRP might improve quality of life and reduce the pain of patients suffering from osteoarthritis of the knee joint independent from the level of cartilage damage.”
PRP vs Hyaluronic Acid
There are 20 PRP studies that show superiority over hyaluronic acid:- The comparison effects of intra-articular injection of Platelet Rich Plasma (PRP), Plasma Rich in Growth Factor (PRGF), Hyaluronic Acid (HA), and ozone in knee osteoarthritis; a one year randomized clinical trial (BMC Musculoskelet Disord. 2021)
- Clinical Efficacy of Platelet-Rich Plasma Injection and Its Association With Growth Factors in the Treatment of Mild to Moderate Knee Osteoarthritis: A Randomized Double-Blind Controlled Clinical Trial As Compared With Hyaluronic Acid (Am J Sports Med. 2021)
- Comparison of two platelet rich plasma formulations with viscosupplementation in treatment of moderate grade gonarthrosis: A prospective randomized controlled study (J Orthop. 2020)
- Single and double-dose of platelet-rich plasma versus hyaluronic acid for treatment of knee osteoarthritis: A randomized controlled trial (World J Orthop. 2019)
- The combined use of platelet rich plasma and hyaluronic acid: prospective results for the treatment of knee osteoarthritis (J Biol Regul Homeost Agents. 2019)
- Intra-articular injections of platelet-rich plasma, hyaluronic acid or corticosteroids for knee osteoarthritis : A prospective randomized controlled study (Orthopade. 2019)
- Intra-articular Injection of Platelet-Rich Plasma Is Superior to Hyaluronic Acid or Saline Solution in the Treatment of Mild to Moderate Knee Osteoarthritis: A Randomized, Double-Blind, Triple-Parallel, Placebo-Controlled Clinical Trial (Arthroscopy. 2019)
- Platelet-Rich Plasma Versus Hyaluronic Acid Injections for the Treatment of Knee Osteoarthritis: Results at 5 Years of a Double-Blind, Randomized Controlled Trial (Am J Sports Med. 2019)
- Clinical therapy of hyaluronic acid combined with platelet-rich plasma for the treatment of knee osteoarthritis (Exp Ther Med. 2018)
- Clinical and radiographic comparison of a single LP-PRP injection, a single hyaluronic acid injection and daily NSAID administration with a 52-week follow-up: a randomized controlled trial (J Orthop Traumatol. 2018)
- Clinical outcomes are associated with changes in ultrasonographic structural appearance after platelet-rich plasma treatment for knee osteoarthritis (Int J Rheum Dis. 2018)
- Knee Osteoarthritis Injection Choices: Platelet- Rich Plasma (PRP) Versus Hyaluronic Acid (A one-year randomized clinical trial) (Clin Med Insights Arthritis Musculoskelet Disord 2015)
- Multiple PRP injections are more effective than single injections and hyaluronic acid in knees with early osteoarthritis: a randomized, double-blind, placebo-controlled trial (Knee Surg Sports Traumatol Arthrosc 2017)
- Intra-Articular Injections of Platelet-Rich Plasma versus Hyaluronic Acid in the Treatment of Osteoarthritic Knee Pain: A Randomized Clinical Trial in the Context of the Spanish National Health Care System (Int J Mol Sci. 2016)
- Randomized controlled trial comparing hyaluronic acid, platelet-rich plasma and the combination of both in the treatment of mild and moderate osteoarthritis of the knee (J Stem Cells Regen Med. 2016)
- Comparison of hyaluronic acid and PRP intra-articular injection with combined intra-articular and intraosseous PRP injections to treat patients with knee osteoarthritis (Clin Rheumatol. 2018)
- Growth Factors Levels Determine Efficacy of Platelets Rich Plasma Injection in Knee Osteoarthritis: A Randomized Double Blind Noninferiority Trial Compared With Viscosupplementation (Arthroscopy. 2018)
- Treatment of knee osteoarthritis: platelet-derived growth factors vs. hyaluronic acid. A
randomized controlled trial (Clin Rehabil. 2018) - Hyaluronic Acid Versus Platelet-Rich Plasma: A Prospective, Double-Blind Randomized Controlled Trial Comparing Clinical Outcomes and Effects on Intra-articular Biology for the Treatment of Knee Osteoarthritis (Am J Sports Med. 2017)
- Platelet rich plasma intra-articular and extra-articular injection for the treatment of knee osteoarthritis (Zhongguo Gu Shang. 2020)
PRP vs Steroid Injections
There are 5 PRP studies that show superiority over steroid injections:
- Intra-articular platelet-rich plasma vs corticosteroids in the treatment of moderate knee osteoarthritis: a single-center prospective randomized controlled study with a 1-year follow up (J Orthop Surg Res. 2020)
- Comparative Effect between Infiltration of Platelet-rich Plasma and the Use of Corticosteroids in the Treatment of Knee Osteoarthritis: A Prospective and Randomized Clinical Trial (Rev Bras Ortop (Sao Paulo). 2020)
- Platelet-Rich Plasma Injections for Advanced Knee Osteoarthritis: A Prospective, Randomized, Double-Blinded Clinical Trial (Orthop J Sports Med. 2017)
- Comparison of Efficiency Between Corticosteroid and Platelet Rich Plasma Injection Therapies in Patients With Knee Osteoarthritis (Arch Rheumatol. 2017)
- Single-dose intra-articular corticosteroid injection prior to platelet-rich plasma injection resulted in better clinical outcomes in patients with knee osteoarthritis: A pilot study (J Back Musculoskelet Rehabil. 2018)
Are you a suitable candidate for PRP?
Research supports that PRP results in knee arthritis decline with severity. PRP works well with mild knee osteoarthritis.Blood Draw Volume
PRP starts with a blood draw from your arm just like giving blood for a diagnostic test. While drawing blood isn’t rocket science, the volumes used here tell an expert quite a bit about the quality of the PRP that the clinic is capable of producing. Why?
Let’s say you’re getting your knee treated at age 50. You show up at the clinic and they take 1 tube of blood to make the PRP. That’s usually about 10 ml.
Your knee will usually take 2-3 ml of PRP. Half of that volume will be wasted, so the PRP that comes out of that process will be at best 2 times more concentrated than the normal platelet concentration in your blood. Hence, without even knowing which PRP kit the clinic is using, since your knee will require at least 10-14X concentration for a real PRP treatment, we know that the clinic is producing inadequate PRP. To get to 2 ml of a 14X PRP, the clinic would have had to take about 6 tubes of blood or 60 ml.
Let’s say you’re getting your knee treated at age 50. You show up at the clinic and they take 1 tube of blood to make the PRP. That’s usually about 10 ml.
Your knee will usually take 2-3 ml of PRP. Half of that volume will be wasted, so the PRP that comes out of that process will be at best 2 times more concentrated than the normal platelet concentration in your blood. Hence, without even knowing which PRP kit the clinic is using, since your knee will require at least 10-14X concentration for a real PRP treatment, we know that the clinic is producing inadequate PRP. To get to 2 ml of a 14X PRP, the clinic would have had to take about 6 tubes of blood or 60 ml.
PRP Processing
That blood taken from your arm now needs to be processed to make PRP. How that happens is critical. 99% of the time, the doctor has bought a kit that goes into a simple bedside centrifuge.There are literally more PRP kits for sale nowadays. Each produces a completely different PRP product. Some of these kits produce junk PRP and some produce high-quality PRP. How would you know?
The other way PRP is processed is through an onsite lab. This could be a very bad or good thing. For example, on the bad side, an improperly run and supervised on-site lab may introduce bacterial contamination or make a bad PRP product. Having said that, a properly supervised and run lab can produce better quality PRP products in more variety than any PRP kit on the market.
PRP Types
There are two main types of PRP and you can tell them by their color-red and amber. Red PRP contains lots of white and red blood cells and is called “Leukocyte Rich” (LR-PRP). Amber PRP has few white and red blood cells, so it’s called “Leukocyte Poor” (LP-PRP).The workhorse of modern PRP use is the amber LP-PRP. Why? While the research bounces back and forth on this one, right now, we have more evidence that amber LP-PRP is more effective for common everyday uses like knee arthritis and tendon problems. However, every rule in medicine has an exception. For the injection of spinal discs (and NOT other areas in the spine), high-dose LR-PRP, based on recent research is likely safer because it helps fight the bacteria that could cause a nasty side effect called discitis.
So unless you’re getting your disc injected, you want the PRP to be amber in color.
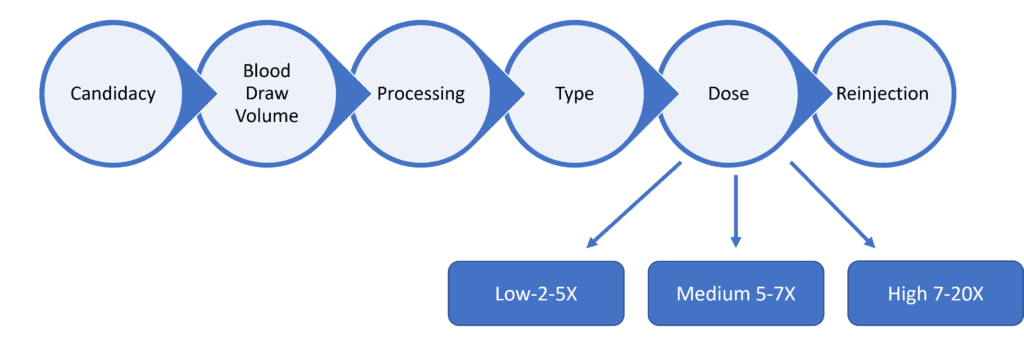
PRP Dose
 |
| Credit: Regenexx.com |
There is nothing in medicine that gets away from the concept of dose. Meaning, if you give the patient the right dose, they get better. If you give the wrong dose, there is no effect. PRP is NO EXCEPTION.
We have tested the concept that the dose of PRP needed is age-dependent numerous times. Meaning younger patients can get by with lower doses. Older patients need much higher doses. How do I know this?
Take our recent published study on tenocytes (tendon cells). When we exposed young tenocytes to PRP they maxed out their ability to heal at low concentrations. However, when old tenocytes were exposed to PRP, the ability to heal was stimulated by a direct dose-response relationship. In other words, the higher the PRP concentration, the more lab-based evidence of healing we observed.
Hence, if you’re young (under the age of 35), you probably don’t need to worry about the PRP dose. However, if you’re middle-aged or older, this is a VERY BIG DEAL that can make the difference between a failed and successful treatment. How high should that dose be?
Based on our published research, if you’re older, this is what we recommend:
- 35-50’s-7-10X PRP
- 50’s-70’s-14X PRP
- 70’s or older-20X PRP
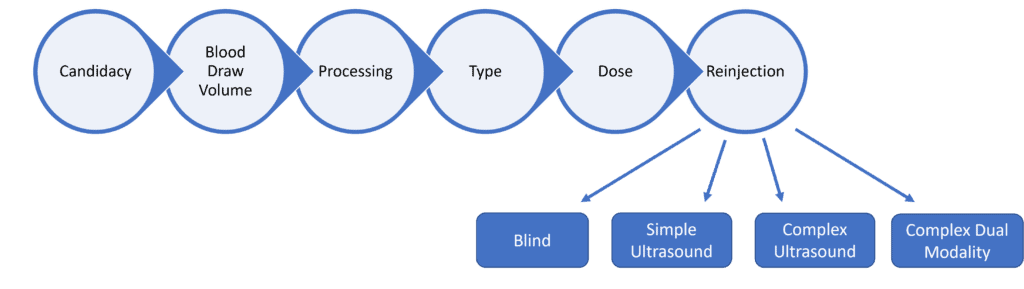
PRP Re-injection
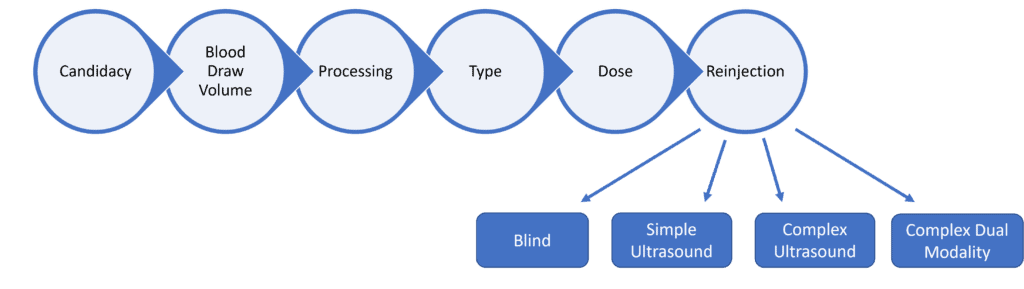
Where the PRP is placed is CRITICAL. Meaning if you want to promote healing in a specific structure, you MUST get the PRP accurately inside that structure.
There are a number of categories here:
- Simple Blind Injections-This means the doctor just pokes the needle in the general vicinity of where it needs to go without using imaging guidance. This is BELOW the current standard of care.
- Simple Ultrasound-guided Injections-The doctor uses an ultrasound machine to guide the needle into an easy to access space like the inside of the knee joint (intra-articular).
- Complex Ultrasound-Guided injections-The doctor is able to use ultrasound to perform more complex injections into specific tendons and ligaments.
- Complex Dual Modality Imaging Injections-The doctor uses both ultrasound and fluoroscopy (x-ray guidance) to be able to perform complex injections in places where ultrasound has poor imaging abilities.
PRP Knee Treatment Cost
The Washington Post reports that knee injections of PRP can cost anywhere from $500 to $1,200 per treatment.
According to the American Academy of Orthopaedic Surgeons, very few insurance plans will provide any reimbursement for PRP injections. The costs must largely be paid out-of-pocket. The costs can also vary from location to location and on how the injections are used.
Insurance companies consider PRP an experimental treatment. More scientific research will have to conclude its effectiveness before it is more widely covered.
Some PRP treatments for knee are also done in combination with add on hyaluronic acid injection.
Hyaluronic acid injection serves to supplement your own hyaluronic acid and keep the bones from scraping against each other. It may also help decrease inflammation and ease pain.
The following medications are types of hyaluronic acid injections:
The following medications are types of hyaluronic acid injections:
- sodium hyaluronate (Euflexxa, Hyalgan, Supartz)
- high-molecular-weight hyaluronan (Monovisc, Orthovisc)
- hylan G-F 20 (Synvisc, Synvisc One)
- cross-liked hyaluronate (Gel-One)
PRP vs Stem Cell Therapy for Knee
There is no one size fits all treatment. There are many options available. On one side of the spectrum are non-invasive strategies such as losing weight and appropriate physical therapy to strengthen your muscles and to have proper walking, standing and sitting habits. In the middle you will have less invasive strategies such as injectables i.e. PRP, steroids, stem cells etc. On the other end of the spectrum are invasive surgical treatments such as bone realignment surgery and total knee replacement (TKR).
PRP might be suitable for stage 1 and 2 knee osteoarthritis and stem cells for stage 2 and 3. Stem cell therapy might not work for Stage 4 knee osteoarthritis.
Discuss with your doctor and choose the least invasive method to begin with.
Key Takeaway
Being a consumer of high-quality healthcare these days takes lots of homework. We hope this guide to high-quality PRP injections helps you find a clinic that has all of the tools needed to help you recover!
Related:
Knee gel injections cost
.png)
.png)

.jpg)

.png)


Comments