The immune system 101: Function, Parts and Boosters 2024
The coronavirus pandemic has turned the world’s attention to the immune system, the body’s defence force against disease-causing bacteria, viruses and other organisms that we touch, ingest and inhale every day.
The system has two types of response in general: innate and adaptive.
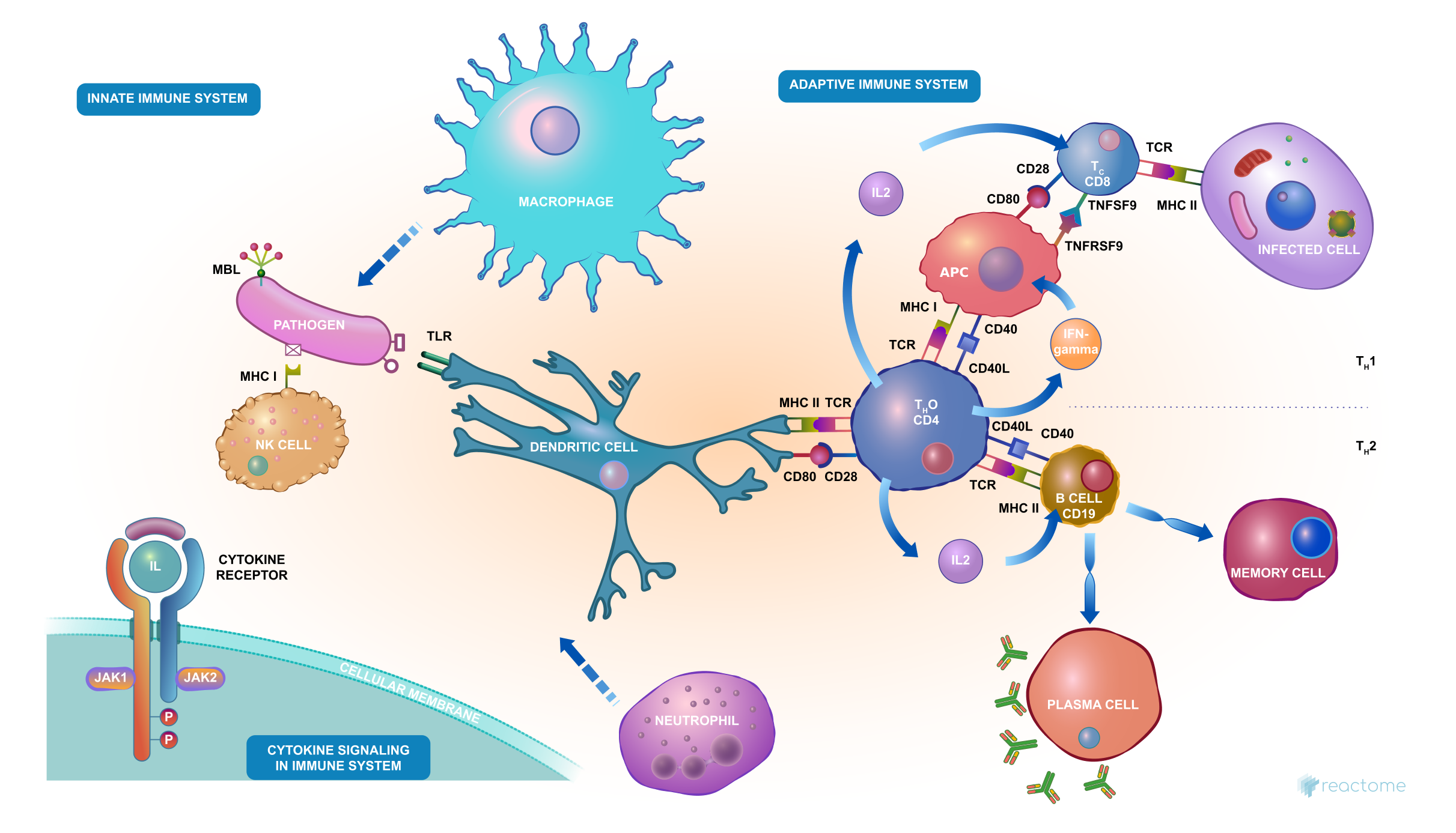
The body’s natural barriers against disease-causing intruders – for example, our skin, the mucous and hairs in our nose, and the acid in our stomachs – are part of our innate immune systems.
Adaptive immunity develops over a lifetime of contact with pathogens and vaccines, preparations which help our immune systems to distinguish friend from foe.
Some infections, like the flu and the common cold, have to be fought many times because so many different viruses or strains of the same type of virus can cause these illnesses. Catching a cold or flu from one virus does not give you immunity against the others.
Friend or foe? The adaptive immune system decides.
Vaccination safely teaches our adaptive immune systems to repel a wide range of diseases, and thus protect ourselves and others.
There is currently no vaccine for coronavirus, and we may not see one for 18 months or longer. So, for now, our immune systems must adapt unaided to this potentially deadly threat.
But the first line of defence is to prevent infection from entering the body.
The World Health Organization’s (WHO) recommended basic protective measures against COVID-19 are frequent handwashing with soap and water, or cleaning hands with an alcohol-based rub; maintaining social distancing; avoiding touching your eyes, nose and mouth; and covering your nose and mouth with a bent elbow or tissue when you cough or sneeze.
These simple actions are vital to slowing the spread of a new disease like the coronavirus – to which nearly everyone is susceptible, but particularly older people and those with underlying health conditions.
There is some evidence that various micronutrient deficiencies — for example, deficiencies of zinc, selenium, iron, copper, folic acid, and vitamins A, B6, C, and E — alter immune responses in animals, as measured in the test tube. However, the impact of these immune system changes on the health of animals is less clear, and the effect of similar deficiencies on the human immune response has yet to be assessed.
So, what can you do? If you suspect your diet is not providing you with all your micronutrient needs — maybe, for instance, you don't like vegetables — taking a daily multivitamin and mineral supplement may bring other health benefits, beyond any possibly beneficial effects on the immune system. Taking megadoses of a single vitamin does not. More is not necessarily better.
Vitamin C
Most people turn to vitamin C after they've caught a cold. That’s because it helps build up your immune system. Vitamin C is thought to increase the production of white blood cells. These are key to fighting infections. Some of the most vitamin C-rich foods include citrus fruits, from tangerines to limes, along with leafy greens, bell peppers and broccoli. Berries are another great source, and they
all provide this and other potent antioxidants, which support your immune response and help to rebuild collagen. Because your body doesn't produce or store it, you need daily vitamin C for continued health. Almost all citrus fruits are high in vitamin C.
On the whole, your immune system does a remarkable job of defending you against disease-causing microorganisms. But sometimes it fails: A germ invades successfully and makes you sick. Is it possible to intervene in this process and boost your immune system? What if you improve your diet? Take certain vitamins or herbal preparations? Make other lifestyle changes in the hope of producing a near-perfect immune response?
But what is the immune system exactly, and how does it help repel intruders?
But what is the immune system exactly, and how does it help repel intruders?
The immune system
The immune system is precisely that — a system, not a single entity. The immune system consists of many inter-related pats working together. Think of it also as the body’s personal army working from the cellular to macro level. Each cell, molecule, tissue and organ in this army plays a vital role in warding off invading pathogens, and also helps guard against internal threats like cancer.The system has two types of response in general: innate and adaptive.
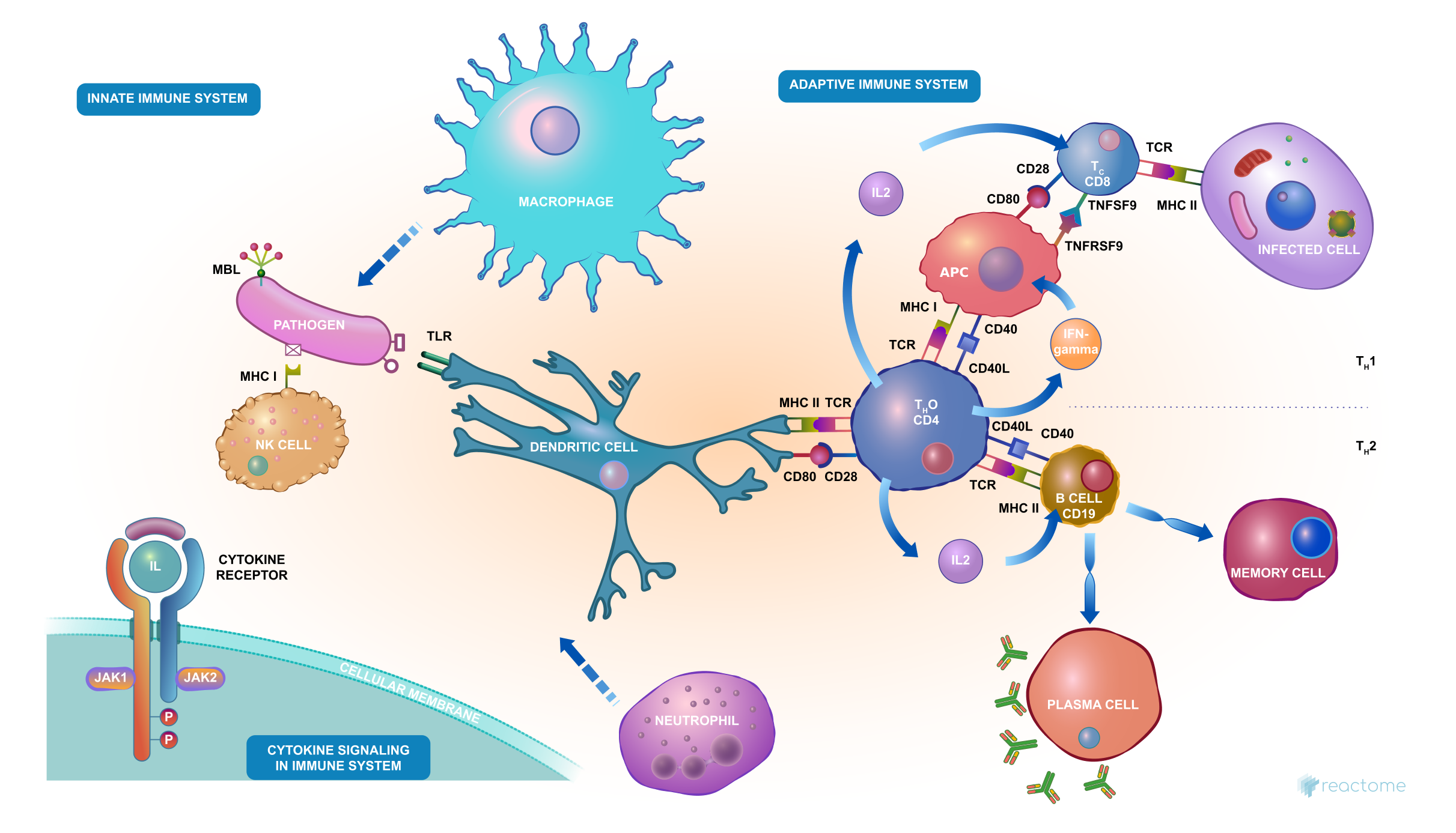
The body’s natural barriers against disease-causing intruders – for example, our skin, the mucous and hairs in our nose, and the acid in our stomachs – are part of our innate immune systems.
Adaptive immunity develops over a lifetime of contact with pathogens and vaccines, preparations which help our immune systems to distinguish friend from foe.
The immune system keeps a record of every microbe it has ever defeated, in types of white blood cells known as memory cells (B and T-lymphocytes). This means it can recognise and destroy the microbe quickly if it enters the body again, before it can multiply and make you feel sick.
Some infections, like the flu and the common cold, have to be fought many times because so many different viruses or strains of the same type of virus can cause these illnesses. Catching a cold or flu from one virus does not give you immunity against the others.
Friend or foe? The adaptive immune system decides.
Vaccination safely teaches our adaptive immune systems to repel a wide range of diseases, and thus protect ourselves and others.
There is currently no vaccine for coronavirus, and we may not see one for 18 months or longer. So, for now, our immune systems must adapt unaided to this potentially deadly threat.
How to boost your immune system
A healthy lifestyle – not smoking, drinking little or no alcohol, sleeping well, eating a balanced diet, taking regular moderate exercise and reducing stress – helps our immune systems to be in the best shape possible to tackle pathogens.But the first line of defence is to prevent infection from entering the body.
The World Health Organization’s (WHO) recommended basic protective measures against COVID-19 are frequent handwashing with soap and water, or cleaning hands with an alcohol-based rub; maintaining social distancing; avoiding touching your eyes, nose and mouth; and covering your nose and mouth with a bent elbow or tissue when you cough or sneeze.
These simple actions are vital to slowing the spread of a new disease like the coronavirus – to which nearly everyone is susceptible, but particularly older people and those with underlying health conditions.
Foods (and the Nutrients Therein) to Boost Your Immune System
Scientists have long recognised that people who live in poverty and are malnourished are more vulnerable to infectious diseases. Whether the increased rate of disease is caused by malnutrition's effect on the immune system, however, is not certain. There are still relatively few studies of the effects of nutrition on the immune system of humans, and even fewer studies that tie the effects of nutrition directly to the development (versus the treatment) of diseases.
So, what can you do? If you suspect your diet is not providing you with all your micronutrient needs — maybe, for instance, you don't like vegetables — taking a daily multivitamin and mineral supplement may bring other health benefits, beyond any possibly beneficial effects on the immune system. Taking megadoses of a single vitamin does not. More is not necessarily better.
Not just vitamins, minerals and phytonutrients, but proteins like collagen and free radical-fighting antioxidants can be introduced to your body through the foods you eat, and play vital roles in helping to keep your body functioning at its best.
In the same way that cross training can keep your body fit and toned by working groups of different muscles, eating a variety of foods will target and work toward healing and restoring many different areas of your body, from your brain to your gut to your immune system.
Protein found in lean meats, bone broth, fish, eggs, nuts and seeds help your body repair tissue and fight infection. Studies show that amino acids in protein, such as arginine and glutamine, increase your body’s ability to heal and decrease inflammation.
In the same way that cross training can keep your body fit and toned by working groups of different muscles, eating a variety of foods will target and work toward healing and restoring many different areas of your body, from your brain to your gut to your immune system.
Protein found in lean meats, bone broth, fish, eggs, nuts and seeds help your body repair tissue and fight infection. Studies show that amino acids in protein, such as arginine and glutamine, increase your body’s ability to heal and decrease inflammation.
Immune System Booster Vitamins and Minerals
Eating foods chock-full of vitamins is an excellent way to strengthen your immune system in order to stay healthy during this pandemic:
Eating foods chock-full of vitamins is an excellent way to strengthen your immune system in order to stay healthy during this pandemic:
- Vitamin A boosts immunity, lowers your risk of infection and supports wound healing through collagen strength. Snack on carrots, squash, sweet potatoes, dark leafy greens, cantaloupe, wild-caught Alaskan salmon, organic pastured eggs and grass fed beef.
- Important for collagen production, zinc is another protective antioxidant that helps create and activate your immune system’s white blood cells and is essential in the enzymatic reactions needed for wound healing. Zinc-containing foods include grass fed red meat (optimal amounts per day range from 5 to 7 ounces), pastured, organic chicken, spinach, nuts and pumpkin seeds.
- Selenium is another powerful antioxidant for immune system protection, found in Brazil nuts and organic, grass fed beef, turkey and chicken. In addition, as important as any food you eat, drinking adequate water is vital for flushing food through your system, flushing toxins and keeping your body hydrated. Many turn to so-called “sports drinks” for hydrating while working out, but clear, pure water is the ideal beverage.
Most people turn to vitamin C after they've caught a cold. That’s because it helps build up your immune system. Vitamin C is thought to increase the production of white blood cells. These are key to fighting infections. Some of the most vitamin C-rich foods include citrus fruits, from tangerines to limes, along with leafy greens, bell peppers and broccoli. Berries are another great source, and they
all provide this and other potent antioxidants, which support your immune response and help to rebuild collagen. Because your body doesn't produce or store it, you need daily vitamin C for continued health. Almost all citrus fruits are high in vitamin C.
Vitamin C appears to be able to both prevent and treat respiratory and systemic infections by enhancing various immune cell functions. Prophylactic prevention of infection requires dietary vitamin C intakes that provide at least adequate, if not saturating plasma levels (i.e., 100–200 mg/day), which optimize cell and tissue levels. In contrast, treatment of established infections requires significantly higher (gram) doses of the vitamin to compensate for the increased metabolic demand. (PubMed).
A large review of 29 studies in 11,306 people demonstrated that regularly supplementing with vitamin C at an average dose of 1–2 grams per day reduced the duration of colds by 8% in adults and 14% in children (PubMed).
Interestingly, the review also demonstrated that regularly taking vitamin C supplements reduced common cold occurrence in individuals under high physical stress, including marathon runners and soldiers, by up to 50% (PubMed, PubMed).
Additionally, high dose intravenous vitamin C treatment has been shown to significantly improve symptoms in people with severe infections, including sepsis and acute respiratory distress syndrome (ARDS) resulting from viral infections (PubMed, PubMed).
For a more comprehensive list of supplements that might help against coronavirus, check out;
can supplements lower your risk with coronavirus?
Vitamin D
A scientific review assessing the specific role vitamin D plays in supporting the immune system’s vital functions shows it directly interacts with the cells that are responsible for fighting infection.
If you're falling ill more often than usual, experiencing cold-like or flu-like symptoms, low vitamin D levels may the underlying cause.
Supporting the link (published in 2014), several large observational studies have found a strong association between a deficiency and respiratory tract infections like colds, bronchitis and pneumonia.
Vitamin D plays a big part in immune health and can be found in limited quantities in raw grass fed milk, wild-caught Alaskan salmon and organic pastured eggs, but the ideal way to optimize your levels is via sunshine.
In a 2019 review of randomized control studies in 11,321 people from 14 countries, supplementing with vitamin D significantly decreased the risk of respiratory infections in people deficient in this vitamin and lowered infection risk in those with adequate vitamin D levels (PubMed).
Other studies note that vitamin D supplements may improve response to antiviral treatments in people with certain infections, including hepatitis C and HIV (PubMed, PubMed, PubMed).
A study that was published in the Journal of the American Geriatrics Society in 2016, revealed that
elderly patients who had high doses of the Vitamin D3 were 40 per cent less likely to develop lung infections. Pneumonia, bronchitis and influenza are known to have higher death rates among older people because of their weakened immune system. Experts believe vitamin D helps to reinforce the first line of defense as people age, to prevent acute respiratory infections.
As for the dosage, anywhere between 1,000 and 4,000 IU of supplemental vitamin D per day is sufficient for most people, though those with more serious deficiencies often require much higher doses (PubMed).
B Vitamins
B vitamins may constitute a long list, but each one is important for different reasons. Other “B’s” for boosting your immunity are especially effective when you combine the foods containing them so they can all work together for maximum effect. These include vitamin B1 (thiamin), B2 (riboflavin), B3 (niacin), B5 (pantothenic acid) and B7 (biotin).
B12, also known as cobalamin, is a powerful cold- and flu-fighting nutrient in your system, as is vitamin B6, another important, germ-combating vitamin that naturally benefits and strengthens your immune system and even protects against the damaging effects of air pollution.
Vitamin B9 and folic acid help repair tissues and aid in cell metabolism and immune support. They’re found in dark leafy greens, wild-caught, cold water fish like herring, mackerel, sardines, anchovies and wild-caught Alaskan salmon, and pastured, organic chicken.
A large review of 29 studies in 11,306 people demonstrated that regularly supplementing with vitamin C at an average dose of 1–2 grams per day reduced the duration of colds by 8% in adults and 14% in children (PubMed).
Interestingly, the review also demonstrated that regularly taking vitamin C supplements reduced common cold occurrence in individuals under high physical stress, including marathon runners and soldiers, by up to 50% (PubMed, PubMed).
Additionally, high dose intravenous vitamin C treatment has been shown to significantly improve symptoms in people with severe infections, including sepsis and acute respiratory distress syndrome (ARDS) resulting from viral infections (PubMed, PubMed).
For a more comprehensive list of supplements that might help against coronavirus, check out;
can supplements lower your risk with coronavirus?
Vitamin D
A scientific review assessing the specific role vitamin D plays in supporting the immune system’s vital functions shows it directly interacts with the cells that are responsible for fighting infection.
If you're falling ill more often than usual, experiencing cold-like or flu-like symptoms, low vitamin D levels may the underlying cause.
Supporting the link (published in 2014), several large observational studies have found a strong association between a deficiency and respiratory tract infections like colds, bronchitis and pneumonia.
Vitamin D plays a big part in immune health and can be found in limited quantities in raw grass fed milk, wild-caught Alaskan salmon and organic pastured eggs, but the ideal way to optimize your levels is via sunshine.
In a 2019 review of randomized control studies in 11,321 people from 14 countries, supplementing with vitamin D significantly decreased the risk of respiratory infections in people deficient in this vitamin and lowered infection risk in those with adequate vitamin D levels (PubMed).
Other studies note that vitamin D supplements may improve response to antiviral treatments in people with certain infections, including hepatitis C and HIV (PubMed, PubMed, PubMed).
A study that was published in the Journal of the American Geriatrics Society in 2016, revealed that
elderly patients who had high doses of the Vitamin D3 were 40 per cent less likely to develop lung infections. Pneumonia, bronchitis and influenza are known to have higher death rates among older people because of their weakened immune system. Experts believe vitamin D helps to reinforce the first line of defense as people age, to prevent acute respiratory infections.
As for the dosage, anywhere between 1,000 and 4,000 IU of supplemental vitamin D per day is sufficient for most people, though those with more serious deficiencies often require much higher doses (PubMed).
B Vitamins
B vitamins may constitute a long list, but each one is important for different reasons. Other “B’s” for boosting your immunity are especially effective when you combine the foods containing them so they can all work together for maximum effect. These include vitamin B1 (thiamin), B2 (riboflavin), B3 (niacin), B5 (pantothenic acid) and B7 (biotin).
B12, also known as cobalamin, is a powerful cold- and flu-fighting nutrient in your system, as is vitamin B6, another important, germ-combating vitamin that naturally benefits and strengthens your immune system and even protects against the damaging effects of air pollution.
Vitamin B9 and folic acid help repair tissues and aid in cell metabolism and immune support. They’re found in dark leafy greens, wild-caught, cold water fish like herring, mackerel, sardines, anchovies and wild-caught Alaskan salmon, and pastured, organic chicken.
"Be Well: A Potential Role for Vitamin B in COVID-19," was published in the February 2021 issue of the journal Maturitas. The paper is the result of a joint collaboration between researchers at the University of Oxford, United Arab Emirates University and the University of Melbourne, Australia.
While no studies using B vitamins have been performed on COVID-19 patients, the researchers stress that, based on B vitamins' effects on your immune system, immune-competence and red blood cells (which help fight infection), supplementation may be a useful adjunct to other prevention and treatment strategies. As noted by the authors:
"There is a need to highlight the importance of vitamin B because it plays a pivotal role in cell functioning, energy metabolism, and proper immune function.
Vitamin B assists in proper activation of both the innate and adaptive immune responses, reduces pro-inflammatory cytokine levels, improves respiratory function, maintains endothelial integrity, prevents hypercoagulability and can reduce the length of stay in hospital.
Therefore, vitamin B status should be assessed in COVID-19 patients and vitamin B could be used as a non-pharmaceutical adjunct to current treatments …
Vitamin B not only helps to build and maintain a healthy immune system, but it could potentially prevent or reduce COVID-19 symptoms or treat SARS-CoV-2 infection. Poor nutritional status predisposes people to infections more easily; therefore, a balanced diet is necessary for immuno-competence."
Garlic
Garlic has shown promise as a treatment for preventing colds and the flu.
Studies have shown that garlic reduces the risk of becoming sick in the first place, as well as how long you stay sick. It can also reduce the severity of symptoms (Trusted Source, Trusted Source).
One study gave 146 healthy volunteers either garlic supplements or a placebo for three months. The garlic group had a 63% lower risk of getting a cold, and their colds were also 70% shorter (Trusted Source).
Another study found that colds were on average 61% shorter for subjects who ate 2.56 grams of aged garlic extract per day, compared to a placebo group. Their colds were also less severe (Trusted Source).
Turmeric and especially its most active compound curcumin have many scientifically-proven health benefits, such as the potential to prevent heart disease, Alzheimer's and cancer. It's a potent anti-inflammatory and antioxidant and may also help improve symptoms of depression and arthritis.
A lab study in 2020 that has yet to be peer-reviewed, demonstrated that Curcumin and other compounds showed promise in blocking the SARS-CoV-2 novel coronavirus from entering cells.
Getting Enough Sleep
Studies show that not getting the sleep you need — for most people eight hours is the minimum for functioning at your best — can compromise your health in ways you may not have considered.
Another study notes that cutting just one hour of sleep a night increases the expression of genes associated with inflammation, immune excitability, diabetes, cancer risk and stress.9 Consistently sleeping less than six hours a night increases your risk for numerous psychological and physical effects. The upshot is, lack of sleep quickly decreases your immune function, leaving your system wide-open for environmental influences, including viruses like colds and flu.
Avoid Sugar
Immune Deficiencies
Immune deficiencies may be temporary or permanent. Temporary immune deficiency can be caused by a variety of sources that weaken the immune system. Common infections, including influenza and mononucleosis, can suppress the immune system.
When immune cells are the target of infection, severe immune suppression can occur. For example, HIV specifically infects T cells, and their elimination allows for secondary infections by other pathogens. Patients receiving chemotherapy, bone marrow transplants, or immunosuppressive drugs experience weakened immune systems until immune cell levels are restored. Pregnancy also suppresses the maternal immune system, increasing susceptibility to infections by common microbes.
Primary immune deficiency diseases (PIDDs) are inherited genetic disorders and tend to cause chronic susceptibility to infection. There are over 150 PIDDs, and almost all are considered rare (affecting fewer than 200,000 people in the United States). They may result from altered immune signaling molecules or the complete absence of mature immune cells. For instance, X-linked severe combined immunodeficiency (SCID) is caused by a mutation in a signaling receptor gene, rendering immune cells insensitive to multiple cytokines. Without the growth and activation signals delivered by cytokines, immune cell subsets, particularly T and natural killer cells, fail to develop normally. The NIAID Primary Immune Deficiency Clinic was established with the goal of accepting all PIDD patients for examination to provide a disease diagnosis and better treatment recommendations.
Read more about PIDDs.
Allergy
Allergies are a form of hypersensitivity reaction, typically in response to harmless environmental allergens like pollen or food. Hypersensitivity reactions are divided into four classes. Class I, II, and III are caused by antibodies, IgE or IgG, which are produced by B cells in response to an allergen. Overproduction of these antibodies activates immune cells like basophils and mast cells, which respond by releasing inflammatory chemicals like histamine. Class IV reactions are caused by T cells, which may either directly cause damage themselves or activate macrophages and eosinophils that damage host cells.
Read more about Allergic Diseases.
Read more about Food Allergy.
Autoimmune Diseases
Autoimmune diseases occur when self-tolerance is broken. Self-tolerance breaks when adaptive immune cells that recognize host cells persist unchecked. B cells may produce antibodies targeting host cells, and active T cells may recognize self-antigen. This amplifies when they recruit and activate other immune cells.
Autoimmunity is either organ-specific or systemic, meaning it affects the whole body. For instance, type I diabetes is organ-specific and caused by immune cells erroneously recognizing insulin-producing pancreatic β cells as foreign. However, systemic lupus erythematosus, commonly called lupus, can result from antibodies that recognize antigens expressed by nearly all healthy cells. Autoimmune diseases have a strong genetic component, and with advances in gene sequencing tools, researchers have a better understanding of what may contribute to specific diseases.
Read more about Autoimmune Diseases.
Sepsis
Sepsis may refer to an infection of the bloodstream, or it can refer to a systemic inflammatory state caused by the uncontrolled, broad release of cytokines that quickly activate immune cells throughout the body. Sepsis is an extremely serious condition and is typically triggered by an infection. However, the damage itself is caused by cytokines (the adverse response is sometimes referred to as a "cytokine storm"). The systemic release of cytokines may lead to loss of blood pressure, resulting in septic shock and possible multi-organ failure.
Read more about Sepsis
Cancer
Some forms of cancer are directly caused by the uncontrolled growth of immune cells. Leukemia is cancer caused by white blood cells, which is another term for immune cells. Lymphoma is cancer caused by lymphocytes, which is another term for adaptive B or T cells. Myeloma is cancer caused by plasma cells, which are mature B cells. Unrestricted growth of any of these cell types causes cancer.
In addition, an emerging concept is that cancer progression may partially result from the ability of cancer cells to avoid immune detection. The immune system is capable of removing infectious pathogens and dangerous host cells like tumors. Cancer researchers are studying how the tumor microenvironment may allow cancer cells to evade immune cells. Immune evasion may result from the abundance of suppressive, regulatory immune cells, excessive inhibitory cytokines, and other features that are not well understood.
References:
Read more: Coronavirus
Disclaimer: No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.
"There is a need to highlight the importance of vitamin B because it plays a pivotal role in cell functioning, energy metabolism, and proper immune function.
Vitamin B assists in proper activation of both the innate and adaptive immune responses, reduces pro-inflammatory cytokine levels, improves respiratory function, maintains endothelial integrity, prevents hypercoagulability and can reduce the length of stay in hospital.
Therefore, vitamin B status should be assessed in COVID-19 patients and vitamin B could be used as a non-pharmaceutical adjunct to current treatments …
Vitamin B not only helps to build and maintain a healthy immune system, but it could potentially prevent or reduce COVID-19 symptoms or treat SARS-CoV-2 infection. Poor nutritional status predisposes people to infections more easily; therefore, a balanced diet is necessary for immuno-competence."
Probiotics
The human microbiome is the trillions of relatively harmless microorganisms (bacteria, fungi, and viruses) that reside on and in the human body. These resident microbes also are referred to as commensals. Scientists are beginning to understand the essential role of the microbiome in human health. Without commensals, the immune system fails to develop properly.
Studies in animal models have shown that commensals play an important role in altering the activity of immune cells, which may lead to different outcomes in disease settings.
The human microbiome is the trillions of relatively harmless microorganisms (bacteria, fungi, and viruses) that reside on and in the human body. These resident microbes also are referred to as commensals. Scientists are beginning to understand the essential role of the microbiome in human health. Without commensals, the immune system fails to develop properly.
Studies in animal models have shown that commensals play an important role in altering the activity of immune cells, which may lead to different outcomes in disease settings.
Probiotics can promote a healthy gut, enhance your immune system and reduce your risk of infection (PubMed, PubMed).
Garlic has shown promise as a treatment for preventing colds and the flu.
Studies have shown that garlic reduces the risk of becoming sick in the first place, as well as how long you stay sick. It can also reduce the severity of symptoms (Trusted Source, Trusted Source).
One study gave 146 healthy volunteers either garlic supplements or a placebo for three months. The garlic group had a 63% lower risk of getting a cold, and their colds were also 70% shorter (Trusted Source).
Another study found that colds were on average 61% shorter for subjects who ate 2.56 grams of aged garlic extract per day, compared to a placebo group. Their colds were also less severe (Trusted Source).
Hydrogen Water
Molecular hydrogen has been shown to have anti-oxidant and anti-inflammatory properties. Yes, we are referring to the hydrogen gas (H2) and not some fancy new chemical entity. It was discovered and reported in Nature in 2007 by a team in Japan, that inhaled hydrogen gas could act as an antioxidant and protect the brain from free radicals. This sparked the interest in its potential health benefits worldwide and led to many published and on-going clinical research.
Published in 2017, a group of researchers in China suggested that hydrogen-rich solution therapy may be a safe, reliable, and effective treatment for Multiple Organ Dysfunction Syndrome (MODS) induced by influenza and other viral infectious diseases (Ref).
A review in 2019 that included 113 references, has also focused on the potential mechanisms of molecular hydrogen against sepsis to provide a theoretical basis for clinical treatment (PubMed).
Quercetin
A study published in 2020 by the University of Tennessee and Oak Ridge National Labs used the most powerful IBM supercomputer to model which FDA approved compounds or supplements might interfere with the coronavirus binding to cells. To review, the coronavirus uses the ACE 2 (Angiotensin Converting Enzyme) receptor to enter cells. Once in a cell, the coronavirus virus empties its RNA contents and hijacks the cell to start producing more viruses. So preventing the coronavirus from binding to the ACE 2 receptor is a good thing as it means the virus can’t get into your cells. The study modeled various compounds and at number 5 on the list as those that has the potential to block the virus was Quercetin.
A 2004 study showed that Quercetin blocked the entry of another SARS coronavirus into cells. A 2012 study basically concluded the same thing (Trusted Source).
This coronavirus is called SARS-CoV-2 and is different from the others in its family. So has Quercetin been shown to do anything that prevents this novel virus from entering cells? A lab study in 2020 that has yet to be peer-reviewed demonstrated that Quercetin and other compounds showed promise in blocking the SARS-CoV-2 novel coronavirus from entering cells.
Molecular hydrogen has been shown to have anti-oxidant and anti-inflammatory properties. Yes, we are referring to the hydrogen gas (H2) and not some fancy new chemical entity. It was discovered and reported in Nature in 2007 by a team in Japan, that inhaled hydrogen gas could act as an antioxidant and protect the brain from free radicals. This sparked the interest in its potential health benefits worldwide and led to many published and on-going clinical research.
Published in 2017, a group of researchers in China suggested that hydrogen-rich solution therapy may be a safe, reliable, and effective treatment for Multiple Organ Dysfunction Syndrome (MODS) induced by influenza and other viral infectious diseases (Ref).
A review in 2019 that included 113 references, has also focused on the potential mechanisms of molecular hydrogen against sepsis to provide a theoretical basis for clinical treatment (PubMed).
Quercetin
A study published in 2020 by the University of Tennessee and Oak Ridge National Labs used the most powerful IBM supercomputer to model which FDA approved compounds or supplements might interfere with the coronavirus binding to cells. To review, the coronavirus uses the ACE 2 (Angiotensin Converting Enzyme) receptor to enter cells. Once in a cell, the coronavirus virus empties its RNA contents and hijacks the cell to start producing more viruses. So preventing the coronavirus from binding to the ACE 2 receptor is a good thing as it means the virus can’t get into your cells. The study modeled various compounds and at number 5 on the list as those that has the potential to block the virus was Quercetin.
A 2004 study showed that Quercetin blocked the entry of another SARS coronavirus into cells. A 2012 study basically concluded the same thing (Trusted Source).
This coronavirus is called SARS-CoV-2 and is different from the others in its family. So has Quercetin been shown to do anything that prevents this novel virus from entering cells? A lab study in 2020 that has yet to be peer-reviewed demonstrated that Quercetin and other compounds showed promise in blocking the SARS-CoV-2 novel coronavirus from entering cells.
Curcumin
Turmeric and especially its most active compound curcumin have many scientifically-proven health benefits, such as the potential to prevent heart disease, Alzheimer's and cancer. It's a potent anti-inflammatory and antioxidant and may also help improve symptoms of depression and arthritis.
A lab study in 2020 that has yet to be peer-reviewed, demonstrated that Curcumin and other compounds showed promise in blocking the SARS-CoV-2 novel coronavirus from entering cells.
Getting Enough Sleep
Studies show that not getting the sleep you need — for most people eight hours is the minimum for functioning at your best — can compromise your health in ways you may not have considered.
Another study notes that cutting just one hour of sleep a night increases the expression of genes associated with inflammation, immune excitability, diabetes, cancer risk and stress.9 Consistently sleeping less than six hours a night increases your risk for numerous psychological and physical effects. The upshot is, lack of sleep quickly decreases your immune function, leaving your system wide-open for environmental influences, including viruses like colds and flu.
If you were looking for a food to eat that would compromise your health in numerous ways and absolutely ruin your health, sugar in its many forms — would win the prize.
To keep your immune system functioning at its best, one of the most effective strategies is to avoid sugar, pure and simple.
To keep your immune system functioning at its best, one of the most effective strategies is to avoid sugar, pure and simple.
Healthy Lifestyle
- Wear protective mask. This is an important public health method to curb the spread. It's not just about protecting yourself but will also protect others from you.
- Abundant evidence suggests that eating whole in fruits, vegetables and whole grains—all rich in networks of naturally occurring antioxidants and their helper molecules—provides protection against free radicals.
- Getting Enough Sleep.
- Avoid Sugar.
- Don't smoke.
- Take steps to avoid infection, such as washing your hands frequently and cooking meats thoroughly.
- Try to minimize stress.
- Drink enough water to keep your body hydrated.
- Avoid excess alcohol.
- Regular physical activity (outdoor activities may not be allowed in countries with 'lock-down').
Disorders of the Immune System
Complications arise when the immune system does not function properly. Some issues are less pervasive, such as pollen allergy, while others are extensive, such as genetic disorders that wipe out the presence or function of an entire set of immune cells.
Immune Deficiencies
Immune deficiencies may be temporary or permanent. Temporary immune deficiency can be caused by a variety of sources that weaken the immune system. Common infections, including influenza and mononucleosis, can suppress the immune system.
When immune cells are the target of infection, severe immune suppression can occur. For example, HIV specifically infects T cells, and their elimination allows for secondary infections by other pathogens. Patients receiving chemotherapy, bone marrow transplants, or immunosuppressive drugs experience weakened immune systems until immune cell levels are restored. Pregnancy also suppresses the maternal immune system, increasing susceptibility to infections by common microbes.
Primary immune deficiency diseases (PIDDs) are inherited genetic disorders and tend to cause chronic susceptibility to infection. There are over 150 PIDDs, and almost all are considered rare (affecting fewer than 200,000 people in the United States). They may result from altered immune signaling molecules or the complete absence of mature immune cells. For instance, X-linked severe combined immunodeficiency (SCID) is caused by a mutation in a signaling receptor gene, rendering immune cells insensitive to multiple cytokines. Without the growth and activation signals delivered by cytokines, immune cell subsets, particularly T and natural killer cells, fail to develop normally. The NIAID Primary Immune Deficiency Clinic was established with the goal of accepting all PIDD patients for examination to provide a disease diagnosis and better treatment recommendations.
Read more about PIDDs.
Allergy
Allergies are a form of hypersensitivity reaction, typically in response to harmless environmental allergens like pollen or food. Hypersensitivity reactions are divided into four classes. Class I, II, and III are caused by antibodies, IgE or IgG, which are produced by B cells in response to an allergen. Overproduction of these antibodies activates immune cells like basophils and mast cells, which respond by releasing inflammatory chemicals like histamine. Class IV reactions are caused by T cells, which may either directly cause damage themselves or activate macrophages and eosinophils that damage host cells.
Read more about Allergic Diseases.
Read more about Food Allergy.
Autoimmune Diseases
Autoimmune diseases occur when self-tolerance is broken. Self-tolerance breaks when adaptive immune cells that recognize host cells persist unchecked. B cells may produce antibodies targeting host cells, and active T cells may recognize self-antigen. This amplifies when they recruit and activate other immune cells.
Autoimmunity is either organ-specific or systemic, meaning it affects the whole body. For instance, type I diabetes is organ-specific and caused by immune cells erroneously recognizing insulin-producing pancreatic β cells as foreign. However, systemic lupus erythematosus, commonly called lupus, can result from antibodies that recognize antigens expressed by nearly all healthy cells. Autoimmune diseases have a strong genetic component, and with advances in gene sequencing tools, researchers have a better understanding of what may contribute to specific diseases.
Read more about Autoimmune Diseases.
Sepsis
Sepsis may refer to an infection of the bloodstream, or it can refer to a systemic inflammatory state caused by the uncontrolled, broad release of cytokines that quickly activate immune cells throughout the body. Sepsis is an extremely serious condition and is typically triggered by an infection. However, the damage itself is caused by cytokines (the adverse response is sometimes referred to as a "cytokine storm"). The systemic release of cytokines may lead to loss of blood pressure, resulting in septic shock and possible multi-organ failure.
Read more about Sepsis
Cancer
Some forms of cancer are directly caused by the uncontrolled growth of immune cells. Leukemia is cancer caused by white blood cells, which is another term for immune cells. Lymphoma is cancer caused by lymphocytes, which is another term for adaptive B or T cells. Myeloma is cancer caused by plasma cells, which are mature B cells. Unrestricted growth of any of these cell types causes cancer.
In addition, an emerging concept is that cancer progression may partially result from the ability of cancer cells to avoid immune detection. The immune system is capable of removing infectious pathogens and dangerous host cells like tumors. Cancer researchers are studying how the tumor microenvironment may allow cancer cells to evade immune cells. Immune evasion may result from the abundance of suppressive, regulatory immune cells, excessive inhibitory cytokines, and other features that are not well understood.
More Information on How Your Immune System Work?
Below is a video-lecture by a medical doctor. Do take note that this lecture was prepared for medical students and might include some technicalities.References:
Read more: Coronavirus
.png)

.png)
.png)

.jpg)




Comments