The Type of Fat You Eat Affects Your COVID Risk
Simply put, unsaturated fat intake is associated with increased mortality from the infection. On the bright side, they believe early treatment with inexpensive calcium and egg albumin will reduce rates of organ failure and ICU admissions.
While no clinical studies have been done yet on this type of therapy, the authors believe it’s time to do one, as it appears early albumin and calcium supplementation can bind unsaturated fats and reduce injury to vital organs. They also point out that saturated fats are protective.
The Most Dangerous Fat of All
I’m currently writing a book on what I believe might be the primary disease-maker in the Western diet, namely omega-6 linoleic acid (LA). And, since diet-related comorbidities are responsible for 94% of all COVID-19-related deaths,2 taking control of your diet is a simple, common-sense strategy to lower the risks associated with this infection.
LA makes up the bulk — about 90% — of the omega-6 consumed and is the primary contributor to nearly all chronic diseases. While an essential fat, when consumed in excessive amounts, LA acts as a metabolic poison.
The reason for this is because polyunsaturated fats such as LA are highly susceptible to oxidation. As the fat oxidizes, it breaks down into harmful sub-components such as advanced lipid oxidation end products (ALES) and OXLAMS (oxidized LA metabolites). These ALES and OXLAMS are actually what cause the damage.
One type of advanced lipid oxidation end product (ALE) is 4HNE, a mutagen known to cause DNA damage. Studies have shown there’s a definite correlation between elevated levels of 4HNE and heart failure.
LA breaks down into 4HNE even faster when the oil is heated, which is why cardiologists recommend avoiding fried foods. LA intake and the subsequent ALES and OXLAMS produced also play a significant role in cancer. HNE and other ALES are extraordinarily harmful even in exceedingly small quantities.
While excess sugar is certainly bad for your health and should typically be limited to 25 grams per day or less, it doesn’t cause a fraction of the oxidative damage that LA does.
Processed vegetable oils are a primary source of LA, but even food sources hailed for their health benefits contain it, and can be a problem if consumed in excess. Cases in point: olive oil and conventionally raised chicken, which are fed LA-rich grains. To learn more about this hidden source of LA, see “Why Chicken Is Killing You and Saturated Fat Is Your Friend.”
Many now understand that your omega-6 to omega-3 ratio is very important, and should be about 1-to-1 or possibly up to 4-to-1, but simply increasing your omega-3 intake won’t counteract the damage done by excessive LA. You really need to minimize the omega-6 to prevent damage from taking place.
LA Damages Your Mitochondria
In order to understand how excess LA consumption damages your metabolism and impedes your body’s ability to generate energy in your mitochondria we need to explore some molecular biology. There’s a particular fat only located in your mitochondria — most of it is found in the inner mitochondrial membrane — called cardiolipin.
Cardiolipin is made up of four fatty acids, unlike triglycerides that have three, but the individual fats can vary. Examples include LA, palmitic acid and the fatty acids found in fish oil, DHA and EPA. Each of these have a different effect on mitochondrial function, and depending on the organ, the mitochondria work better with particular kinds of fatty acids.
For example, your heart preferentially builds cardiolipin with LA, while your brain dislikes LA and preferentially builds cardiolipin in the mitochondria with fats like DHA. As mentioned, LA is highly susceptible to oxidation.
The LA within the mitochondria cardiolipin is exposed to cytochromes in the electron transport chain that contain iron, which in turn can catalyze oxidation of the cardiolipin. This is bad news because oxidation of cardiolipin is one of the things that controls autophagy.
In other words, oxidation of cardiolipin is one of the signals your body uses when there’s something wrong with a cell, so it triggers the destruction of that cell, a process called apoptosis. Your cells know that they’re broken when they have too many damaged mitochondria, and the process that controls this is largely the oxidation of omega-6 fats contained within cardiolipin.
So, by altering the composition of cell membranes and stored fatty acids in cells to one that's richer in omega-6 fats, you make your cardiolipin far more susceptible to oxidative damage. The good news is that by making a few well-chosen tweaks to your diet, you change the composition of fatty acids in both your cell membranes and your cardiolipin to a favorable composition.
Fat Intake Linked to COVID-19 Outcomes
Getting back to the issue of how your fat intake can affect your COVID-19 outcome, the Gastroenterology paper3 points out that unsaturated fats “cause injury [and] organ failure resembling COVID-19.” More specifically, unsaturated fats are known to trigger lipotoxic acute pancreatitis, and the sepsis and multisystem organ failure seen in severe cases of COVID-19 greatly resembles this condition.
The solution they propose, namely early supplementation with egg albumin and calcium, is thought to be helpful because they are known to bind unsaturated fats, thereby reducing injury to organs. The two conditions also share other risk factors. As explained in the paper:4
“Unsaturated fatty acids (UFAs) generated by adipose lipolysis cause multisystem organ failure, including acute lung injury. Severe acute pancreatitis and severe COVID-19 share obesity as a risk factor, along with lipase elevation, hypoalbuminemia, and hypocalcemia.”The authors further explain that the ACE2 receptor that the SARS-CoV-2 virus uses to gain entry into your cells resides on fat cells, and oleic acid — a monounsaturated omega-9 fat found in olive oil — has been shown to cause multisystem organ failure, including acute lung injury.
PUFAs in general also depolarize mitochondria and increase inflammatory mediators. All of this is what caused the researchers to explore the potential connection between lipotoxicity (toxicity caused by harmful fats such as LA) and severe COVID-19 resulting in organ failure.
Saturated fat intake (kg/capita/y) was negatively associated, and percent unsaturated fatty acid intake was positively associated with [COVID-19] mortality. ~ Gastroenterology September 2020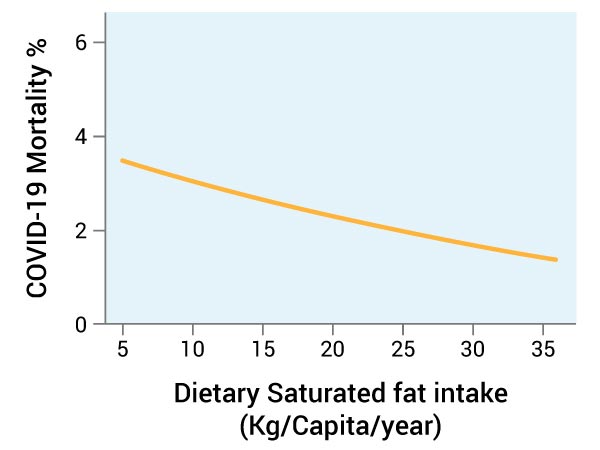
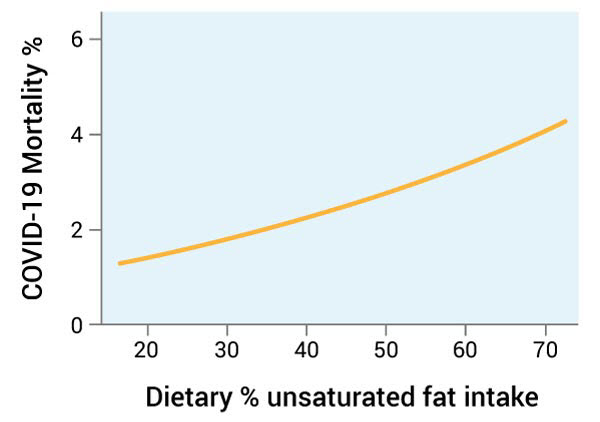
The paper contains an interesting diagram that summarizes the investigative approach they took to reach the conclusion that unsaturated fat intake correlates to COVID-19 outcomes, which I unfortunately cannot include here. In summary, though, it shows that higher intakes of polyunsaturated fats (PUFAs), primarily LA, resulted in a greater risk of severe COVID-19, while higher intake of saturated fat lowered the risk.
PUFAs Raise COVID-19 Mortality While Saturated Fat Lowers It
The researchers discovered that hypocalcemia (lower-than-average levels of calcium in your blood or plasma) and hypoalbuminemia (low albumin in your blood) are observable early on in patients with severe COVID-19.
When looking at data from COVID-19 patients, the also found that low arterial partial pressure of oxygen and percentage of oxygen ratios were associated with higher levels of unbound fatty acid levels in their blood. They also speculate that UFAs may cause vascular leakage, inflammatory injury and arrhythmia during severe COVID-19.
In tests on mice, animals given LA developed a range of conditions resembling lethal COVID-19, including hypoalbuminemia, leucopenia (low white blood cell count), lymphopenia (low lymphocyte count), lymphocytic injury, thrombocytopenia (low platelet count), hypercytokinemia (cytokine storm), shock and kidney failure.
How to Calculate Your LA Intake With Cronometer
Considering the damage LA imparts, it’s not surprising that it could play a significant role in the outcome of COVID-19. As mentioned, virtually all of the comorbidities associated with COVID-19 are diet related, share many of the same risk factors, and can be triggered or worsened by high LA intake.
Fortunately, you won’t have to spend hundreds of dollars to have your food analyzed for LA. All you need to do is accurately enter your food intake into Cronometer — a free online nutrition tracker — and it will provide you with your total LA intake. The key to accurate entry is to carefully weigh your food with a digital kitchen scale so you can enter the weight of your food to the nearest gram.
cronometer.com is free to use when you use the desktop version. If you feel the need to use your cellphone (which is not recommended) to enter your data, then you will need to purchase a subscription. Personally, I have used the desktop version exclusively for the last five years as it has greater functionality and allows me to avoid electromagnetic fields from my phone.
Ideally, it is best to enter your food for the day before you actually eat it. The reason for this is quite simple: It’s impossible to delete the food once you have already eaten it, but you can easily delete it from your menu if you find something pushes you over the ideal limit.
Once you’ve entered the food for the day, go to the “Lipid” section on the lower left side of the app. The image below is taken from one of my recent data entries and shows you what the section looks like. To find out how much LA is in your diet for that day, you merely need to see how many grams of omega-6 is present. About 90% of the omega-6 you eat is LA.
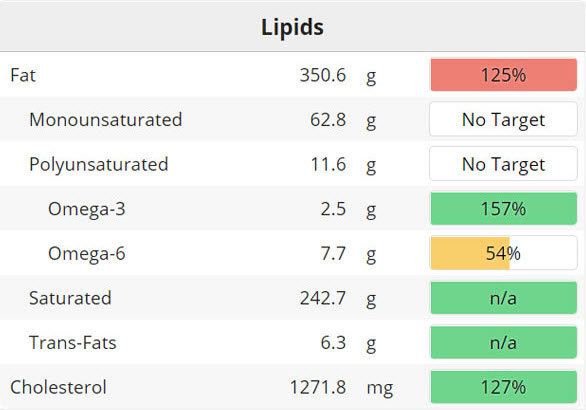
To find out the percentage of calories the omega-6/LA represents in your diet, go to the “Calories Summary” section shown in the image below. In my case, I consumed 3,887 calories. Since there are nine calories per gram of fat, you will need to multiply the number of omega-6 grams times nine to obtain the total amount of omega-6 calories. In my case, that is 69.3 calories.
Next, divide the LA calories by your total calories. In this example, that would be 69.3/3887 = .0178. If you multiply that number by 100, or move the decimal point two spaces to the left, you will have the percentage as a whole number. In my example, it is 1.8% of LA. This falls within the ideal LA percentage range, which is between 1% and 2% of your total calorie intake.
Cronometer is in the process of automatically displaying the “Percent of Omega-6” in your diet, but that will not be deployed until early 2021, so use the formula above to calculate it for yourself until then.
Helpful Feature You Might Not Be Aware Of
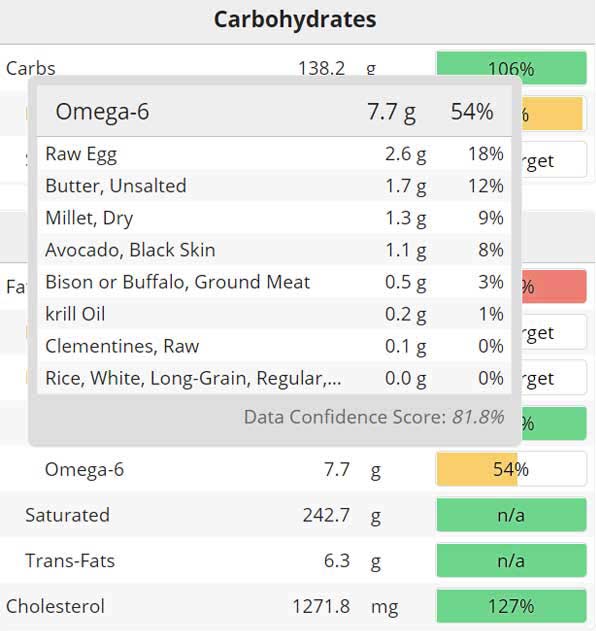
Most people aren’t aware of an incredibly helpful feature in Cronometer that allows you to easily identify where all your LA is coming from. If you mouse over the percent field next to the omega-6 value, you will see a popup displayed that will rank order the foods based on the quantity of LA they contain.
In my case, below, you can see that the four eggs I ate are my largest source of LA. Eggs are a very healthy food but, unfortunately, nearly all chickens, including pasture raised, are fed grains that are loaded with LA. Even if the grains are organic, they still contain LA.
I raise my own chickens and am in the middle of an experiment to change this by feeding my chickens a very low-LA, no-grain diet. I will have the eggs analyzed in a research lab and hope to get the LA levels 90% lower, which should hopefully get my LA intake below 5 grams.
It is interesting to note from my analysis that my primary protein, bison, only contributes 0.5 grams of LA even though I had 8 ounces that day. For the most part, fruit is also LA-free, which makes it a better source of healthy carbs than grains.
I also use rice on my high-carb diet days, in this case about 100 grams of carbs for the day, and the rice has no LA in it. Both rice and millet are two of the best grains to use as they have no gluten. The rice has the additional advantage, though, of being LA-free. It is best to use white rice, as the fiber in brown rice provides little nutritional benefit and may actually cause some problems.
Carbohydrates — Choose Wisely
I must admit that I have a prejudice in this area as my first book in 2004 (which was a New York Times best seller) was “The No Grain Diet.” The concern about avoiding grains was largely based on consuming excessive carbohydrates that could lead to insulin resistance. At the time, I wasn’t aware that increased LA consumption was likely a far more significant issue than excessive carbs, or that most grains are typically loaded with LA.
However, when you have increased carbs in the form of sugar and processed wheat, and then add seed oils, you have the Devil’s Triad, which collectively contribute to most metabolic diseases.
So even though I wrote the book 17 years ago, I still believe most grains should be avoided, or at the least minimized, because they are typically high in carbs and LA. Many are also loaded with other problems like gluten, oxalates and phytates.
In my more recent book, “Fat for Fuel,” I advocated the cyclical use of balanced and healthy carbs in the form of fruits and healthier grains. For most of us, fruit is a far healthier option than grains as there is virtually no LA in fruit, with exceptions like avocado, which is technically a fruit.
Metabolic Flexibility Is Key for Optimal Health
About 90% of the population is insulin resistant. Ideally, you will first want to become metabolically flexible and improve your ability to burn fat as your primary fuel. I discuss this strategy extensively in “Fat for Fuel.” It typically takes a few weeks to a few months for someone to transition to a metabolically flexible state.
When you are metabolically flexible, you will typically have normal blood pressure, not be overweight, and have a fasting blood glucose below 90, which you can easily measure at home.
While limiting carbs to less than 50 grams per day when you are metabolically inflexible is a powerful strategy, once you regain your ability to burn fat for fuel, most will find that they need to include a healthy source of carbs back into their diet. A simple strategy would be to shoot for around 50 grams on your low-carb days and double or triple that on your high-carb days.
You can start by simply alternating low and high carb days and monitor your fasting blood glucose. If it starts to rise over time, you will know that it is probably better to decrease the frequency of your high-carb days. Again, the best carbs to use would be fruit or white rice, as they are virtually LA-free. After you have been on a low-LA diet for a year or two, you can integrate other carbs that are higher in LA.
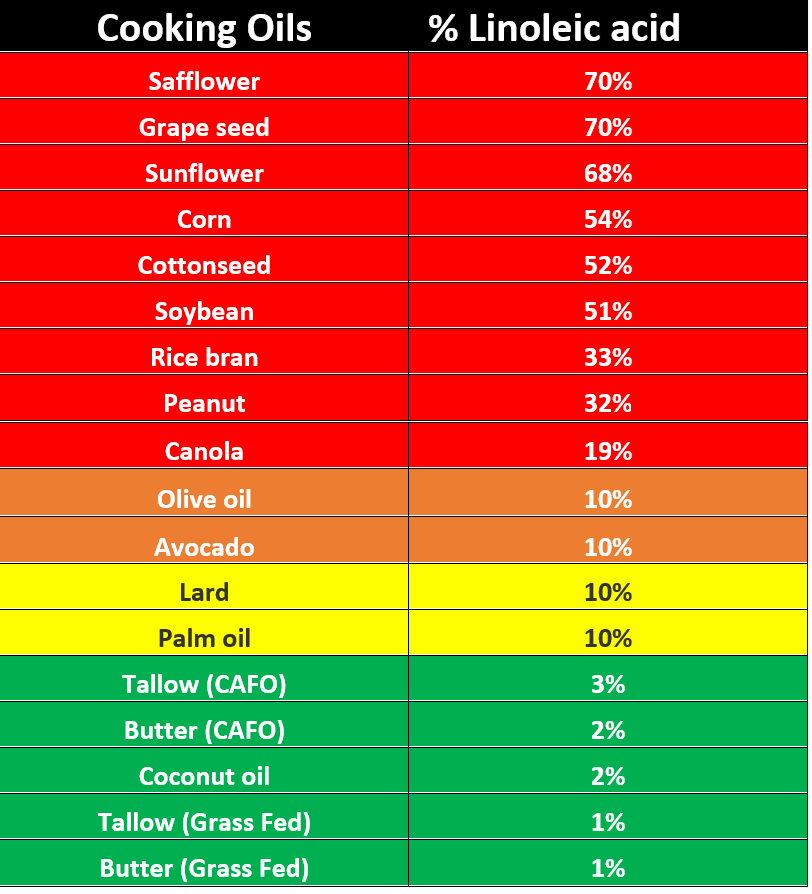
Fats — Be Careful of Cooking Oils
Ideally, it would be best to limit the amount of oil you use for cooking. Typically, it is better to cook using no oils and substitute grass-fed butter, instead. This is because seed oils are the single greatest source of omega-6 LA and the higher you heat food, the more toxic byproducts you create.
You might wonder how you can limit your cooking oils. Let me give you an example. If you were cooking ground beef or bison, you could cook in a frying pan or in a covered pot over low heat using the water in the meat to convert to steam and cook the food at a low 212 degrees Fahrenheit.
If you choose to use oil for cooking, then you can use the table5 below to help you select the best oils. It is color coded to guide you. The preferred oils are shaded green. Notice that concentrated animal feeding operation (CAFO) beef tallow or butter has three times as much LA as the grass-fed version.6 They still are very low and within an acceptable range, but it is clearly better to choose the higher quality grass fed version when you can.
Lard and palm oil are less preferred options because of their higher LA content. There is a load of confusion around olive oil, though, that needs to be cleared up. And, while avocado oil isn’t widely appreciated, it too has the same concerns as olive oil.
Both olive oil and avocado oil LA content varies widely. Typically, it will average around 10%, although some oils could be twice as high. The reason one needs to be ultra-careful using these oils is because the vast majority (over 80%) are adulterated with cheaper and high LA oils like safflower.
So, if you plan on using either of these oils, you need to have independent objective confirmation that the oil has not been tampered with. These brands are typically more expensive as authentic olive and avocado oils have much higher production costs.
Oils that should be completely avoided at all times are the primary culprits of destroying health in the 20th century: the toxic seed oils that are shaded in red. That said, the dose makes the poison. So, you can theoretically use any of the oils in the table below so long as your total intake of LA for that day is less than 2% of your total calories. The higher up on the table the oil is, the more likely you will exceed your safe limit for the day.
What About Seeds and Nuts?
Seeds and nuts can be used in moderation. The table below indicates approximately how much LA is common seeds7 and nuts.8,9, 10 You can see that most are nearly half LA. For that reason, it is very easy to reach really high levels of LA if you eat lots of seeds and nuts, with the exception of macadamia nuts.
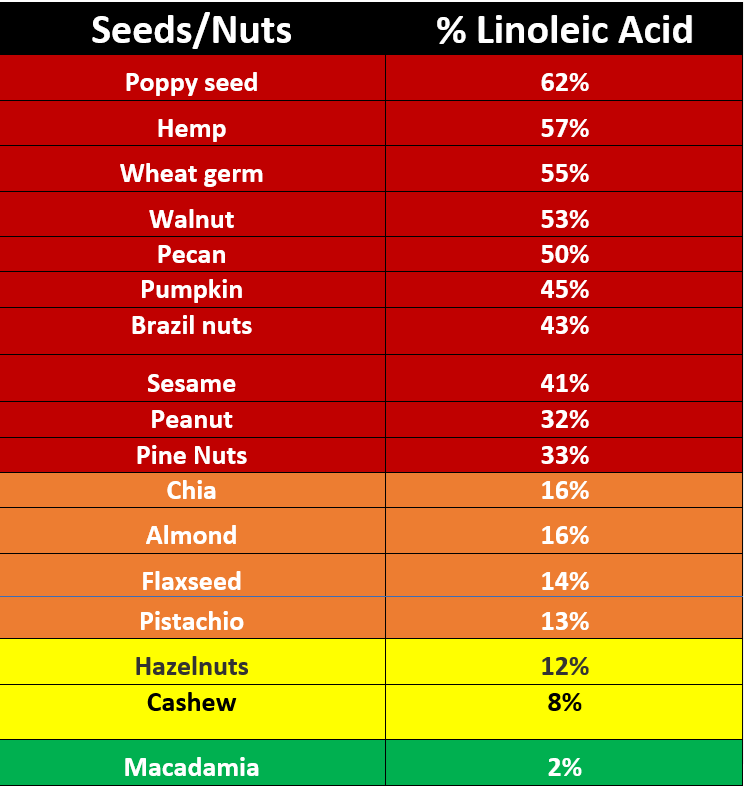
Also keep in mind that even if the nut has a relatively low quantity of LA, like almonds, it could be loaded with other potential problems like oxalates. Oxalates are razor sharp crystals contained in many nuts and seeds. They are water soluble and only found in the unprocessed seed or nut. If you are consuming an oil version of the seed or nut, it will contain virtually no oxalates.
So, the key here is that seeds and nuts are clearly allowed, but large quantities should be avoided. Be sure to enter them into Cronometer so you can see precisely how much LA they contain and how they are influencing your total daily intake.
Please note that the percent of LA indicated for the foods above is the typical average. It is important to understand that the percent of LA in any specific food can be highly variable based on many factors, but the values listed are what are typically found in the literature.
Ideal Sources of Protein
In general, animal foods are typically much lower in LA than vegetable sources. This is especially true for seeds and most all nuts, except macadamia, as you can see in the table above. Additionally, many vegetable sources have oxalates, phytates and gluten, which have been previously well-documented to have adverse health effects.
There are two important exceptions, though. Ideally, you will want to limit your intake of chicken and pork as these animals are universally fed grains that are loaded with LA. It is common for them to have LA levels from 10% to 20%. They will contain lower amounts of LA if they are not raised in a factory farm (CAFO), but most likely will exceed levels in lamb, beef, bison and other game animals like elk, by 10-fold.
For most of us, the ideal source of protein would be from bison, followed by beef and lamb. An 8-ounce serving of these foods typically has less than 1 gram of LA. In addition to eating muscle meat, it would be wise to regularly include sources of organ meats, as they are loaded with important micronutrients not found in muscle meat.
Eggs are another source of LA concern as the yolks are about 16% LA. This is because nearly all chickens, including those that are pasture raised, are given grain as their primary feed. As long as you aren’t allergic to eggs, they are an incredibly healthy nutrient-dense food and one of the finest sources of bioavailable choline available.
I believe it would be wise to limit eggs to four or less per day, as that would provide about 2.5 grams of LA. As mentioned earlier, I am currently in the middle of an experiment.
I’m feeding my 20 chickens a low-LA carnivore-type diet consisting of 1 gallon of 4-day-old sprouted mung beans with 4 ounces of melted butter mixed in, along with a regular supply of beef liver and mealworms. I will be analyzing the eggs for LA in the next few months as it takes some time for LA to be liberated after it’s consumed.
- 1, 3, 4 Gastroenterology 2020 Sep; 159(3): 1015–1018.e4
- 2 CDC.gov August 26, 2020
- 5 Chempro Fatty Acid Composition of Oils and Fats
- 6 Weston A Price Fatty Acid Analysis of Grass-fed and Grain-fed Beef Tallow
- 7 Journal of the American Oil Chemists' Society. 72 (9): 1079–1081
- 8 Li, D., & Hu, X. (2011). Fatty Acid Content of Commonly Available Nuts and Seeds. Nuts and Seeds in Health and Disease Prevention, 35–42.
- 9 British Journal of Nutrition 96 Suppl 2(S2): S29-35
- 10 The Paleo Diet Seed Fatty Acid Composition
.png)
.png)


.png)
.jpg)



Comments