Vitamin D 101: Deficiency Symptoms, Benefits, Sources, and Side Effects (2024)
Vitamin D, or the “sunshine vitamin,” is considered both a fat-soluble vitamin and a hormone because it can be obtained nutritionally, and our skin can synthesize it through sunlight exposure. It is integral to various bodily functions.
Primarily recognized for enhancing calcium absorption, vitamin D plays a role in maintaining bone and dental health, supporting the immune system, regulating cell growth, influencing mood, and preventing conditions such as multiple sclerosis.

Vitamin D2 is known as ergocalciferol. It is found in some plants, mushrooms, and yeasts.
The RDI for Vitamin D is as follows (nih.gov):
400 IU (10 mcg): infants, 0–12 months
600 IU (15 mcg): children and adults, 1–70 years old
800 IU (20 mcg): older adults and pregnant or breastfeeding women
According to the U.S. National Academy of Medicine, the safe upper limit is 4,000 IU (100 mcg) per day (nih.gov).
However, don’t consume more than 4,000 IU of vitamin D without your doctor’s permission. It exceeds the safe upper limits of intake and is not linked to more health benefits (Trusted Source).
Many of vitamin D health benefits have been thoroughly confirmed in the biomedical literature. In fact, since 1964, there have been more than 100,000 search results on PubMed database (National Library of Medicine).
We have compiled and organised salient research in this article, on well over 20 health conditions (including COVID-19) that may be benefited from the use of vitamin D.
ii. Vitamin D and Psoriasis
Oral Vitamin D supplementation is an important supplementary therapeutic choice for psoriatic patients. Vitamin D supplementation may also be crucial in preventing psoriasis-related comorbidities, hypertension and metabolic syndromes.
It’s still uncertain if high-dose supplementation provides any benefits for long-term patients with vitiligo.
This is likely because vitamin D gets the calcium into the blood, then vitamin K tells the calcium where it is most needed.
Taking vitamin D3 and K2 together actually promotes new bone growth. In 2019, researchers observed that vitamin D3 and K2 worked in tandem to form new osteoblasts, the cells that secrete osteocalcin, which is a biomarker for new bone growth.
Deficiency is also linked to osteoporosis, reduced mineral density, and increased risk of falls and fractures in older adults (Source).
The main symptoms of toxicity include confusion, lack of concentration, drowsiness, depression, vomiting, abdominal pain, constipation, and high blood pressure (Trusted Source). Other side effects of Vitamin D include..
While an increasing number of people are supplementing with vitamin D, it’s rare to find someone with very high blood levels of this vitamin.
One recent study looked at data from more than 20,000 people over a 10-year period. It found that only 37 people had levels above 100 ng/ml (250 nmol/l). Only one person had true toxicity, at 364 ng/ml (899 nmol/l) (Trusted Source).
In one case study, a woman had a level of 476 ng/ml (1,171 nmol/l) after taking a supplement that gave her 186,900 IU of vitamin D3 per day for two months.
This was a whopping 47 times the generally recommended safe upper limit of 4,000 IU per day. The woman was admitted to the hospital after she experienced fatigue, forgetfulness, nausea, vomiting, slurred speech, and other symptoms.
Although only extremely large doses can cause toxicity so rapidly, even strong supporters of these supplements recommend an upper limit of 10,000 IU per day (Trusted Source).
Symptoms of hypercalcemia, or high blood calcium levels, include:
In one case study, an older man with dementia who received 50,000 IU of vitamin D daily for 6 months was repeatedly hospitalized with symptoms related to high calcium levels (Trusted Source).
In another, two men took improperly labeled vitamin D supplements, leading to blood calcium levels of 13.2–15 mg/dl (3.3–3.7 mmol/l). What’s more, it took a year for their levels to normalize after they stopped taking the supplements (Trusted Source).
One study followed 10 people who had developed excessive calcium levels after they had taken high-dose vitamin D to correct deficiency. Four of them experienced nausea and vomiting, and three of them had a loss of appetite (Trusted Source).
Similar responses to vitamin D megadoses have been reported in other studies. One woman experienced nausea and weight loss after taking a supplement that was found to contain 78 times more vitamin D than stated on the label (Trusted Source, Trusted Source).
Importantly, these symptoms occurred in response to extremely high doses of vitamin D3, which led to calcium levels greater than 12 mg/dl (3.0 mmol/l).
These symptoms may occur in those receiving high doses of vitamin D to correct deficiency. As with other symptoms, response appears to be individualized even when vitamin D blood levels are similarly elevated.
One of vitamin K2’s most important functions is to keep calcium in the bones and out of the blood. It’s believed that very high vitamin D levels may reduce vitamin K2 activity (Trusted Source, Trusted Source).
To protect against bone loss, avoid taking excessive vitamin D supplements and take a vitamin K2 supplement. You can also eat foods rich in vitamin K2, such as grass-fed dairy and meat.
In one case study, a man was hospitalized for kidney failure, elevated blood calcium levels, and other symptoms that occurred after he received vitamin D injections prescribed by his doctor (Source).
Indeed, most studies have reported moderate-to-severe kidney injury in people who develop vitamin D toxicity (Trusted Source, Trusted Source, Trusted Source, Trusted Source, Trusted Source, Trusted Source).
In one study in 62 people who received excessively high-dose vitamin D injections, each person experienced kidney failure — whether they had healthy kidneys or existing kidney disease (Trusted Source). Kidney failure is treated with oral or intravenous hydration and medication.
Calcitriol interacts with the vitamin D receptor (VDR), which is found in almost every single cell in your body (Trusted Source, Trusted Source). When the active form of vitamin D binds to this receptor, it turns genes on or off, leading to changes in your cells. This is similar to how most other steroid hormones work (Trusted Source, Trusted Source).
Those who are at high risk of having low levels of vitamin D include:
Your doctor will tell you not to eat anything for four to eight hours before the test.
Results will depend on your age, sex, and the testing methods used. Results can also slightly vary from lab to lab.
According to the Office of Dietary Supplements (ODS), levels of vitamin D are measured by the 25-hydroxy level in nanomoles/liter (nmol/L) or nanograms/milliliter (ng/mL). The results can indicate the following:
Low blood levels of 25-hydroxy vitamin D usually mean one (or more) of the following:
As with any routine blood test, risks of the 25-hydroxy vitamin test are minimal and include excessive bleeding, lightheadedness and a slight chance of infection where the needle pierces your skin.
Primarily recognized for enhancing calcium absorption, vitamin D plays a role in maintaining bone and dental health, supporting the immune system, regulating cell growth, influencing mood, and preventing conditions such as multiple sclerosis.
Contents
- What is Vitamin D
- Types of Vitamin D
- Vitamin D Dosage
- Benefits of Vitamin D
- Vitamin D Foods
- Vitamin D and Other Supplements
- Vitamin D Deficiency Symptoms
- Side Effects of Vitamin D
- How To Measure Vitamin D Levels
- Vitamin D Interactions with other Medications and Supplements
- Online Shopping Guide
1. What is Vitamin D
Vitamin D or known as “calciferol” is a fat-soluble vitamin that can be found naturally in certain types of food. Sunlight is also a natural source of Vitamin D. Our skin produces Vitamin D when exposed to the sun’s ultraviolet B (UVB) rays.
They are also sold in the form of dietary supplements.
Related: Best Vitamin D Supplements
a. How the Body Processes Vitamin D – Vitamin D activation

Vitamin D needs to undergo two conversion steps to become active (Source, Source).
First, it is converted to calcidiol, or 25(OH)D, in your liver. This is the storage form of the vitamin.
First, it is converted to calcidiol, or 25(OH)D, in your liver. This is the storage form of the vitamin.
Second, it is converted to calcitriol, or 1,25(OH)2D, mostly in your kidneys. This is the active, steroid-hormone form of vitamin D.
b. What Does Vitamin D Do In Your Body?
Calcitriol interacts with the vitamin D receptor (VDR), which is found in almost every single cell in your body (Trusted Source, Trusted Source).
When the active form of vitamin D binds to this receptor, it turns genes on or off, leading to changes in your cells. This is similar to how most other steroid hormones work (Trusted Source, Trusted Source).
When the active form of vitamin D binds to this receptor, it turns genes on or off, leading to changes in your cells. This is similar to how most other steroid hormones work (Trusted Source, Trusted Source).
c. How Long is Vitamin D Stored in the Body?
Vitamin D undergoes two hydroxylations in the body for activation. Calcitriol (1,25-dihydroxyvitamin D3), the active form of Vitamin D, has a half-life of about 15 h, while calcidiol (25-hydroxyvitamin D3) has a half-life of about 15 days. (Source)2. Types of Vitamin D
Vitamin D is more than just one vitamin. It’s a family of nutrients that shares similarities in chemical structure.
a. Vitamin D2 vs Vitamin D3
Vitamin D3 is also known as cholecalciferol. It is found in some animal foods, like fatty fish and egg yolks. Your skin makes vitamin D3 when it’s exposed to sunlight.
Vitamin D2 is known as ergocalciferol. It is found in some plants, mushrooms, and yeasts.
Both are effectively absorbed into the bloodstream. However, the liver metabolizes them differently.
Vitamin D3 (cholecalciferol) is found to be almost twice as effective at increasing the blood levels of Vitamin D compared to Vitamin D2 (ergocalciferol) (Source, Source).
Vitamin D2 supplements are created by subjecting a plant sterol to ultraviolet energy, resulting in the production of vitamin D2. Vitamin D3 is usually generated through the irradiation of 7-dehydrocholesterol derived from lanolin obtained from sheep’s wool. Individuals who abstain from all animal-derived products can ask manufacturers about supplement sourcing and processing methods.
Ongoing debate surrounds the preference for vitamin D3 over D2 to increase blood levels. A meta-analysis suggests that D3 supplements tend to raise and maintain vitamin D levels more effectively than D2. Many experts favor vitamin D3 due to its natural production in the body and its presence in foods containing the vitamin.
One study involving 15,716 participants compared four treatment options for vitamin D deficiency, including vitamin D2 injection, vitamin D3 injection, a combination of vitamin D2 injection with a D2 tablet, and a combination of vitamin D3 injection with a D2 tablet. All treatments led to a significant increase in serum vitamin D within 12 weeks, with the vitamin D3 injection alone showing the highest increase. The findings suggest that using vitamin D3 in injectable form is the most effective option for restoring severe vitamin D deficiency, outperforming the injectable form of vitamin D2 and D2 tablets. However, the study did not address the effects of a vitamin D3 tablet/capsule, which is still generally better absorbed than oral vitamin D2.
b. Liposomal Vitamin D3
Liposomal Vitamin D3 may offer a greater potential for improved bioavailability over regular non-liposomal vitamin D3. The added phospholipids from non-soy sunflower lecithin contribute to a more efficient and ideal absorption of Vitamin D.
Traditional vitamin D does not have the same potential for bioavailability advantages. Non-liposomal vitamin D is absorbed through your intestinal tract in a much different way.
In the intestine, vitamin D..
- Must be first broken down by your digestive system.
- Once broken down into smaller fragments, they can be absorbed.
- The nutrients enter your bloodstream for your body to use.
But with liposomal technology, you don’t have to depend on your GI tract to process the vitamin D3 molecules before they can be absorbed. Liposomes surround many of the vitamin D3 molecules with a cellular membrane-like coating, allowing vitamin D3 to slip across the gut membrane.
i. How Liposomal Vitamin D3 Works
- After swallowing the capsule, it travels into your stomach and intestines.
- The acids in your stomach cause the capsule to rapidly disintegrate and release its contents.
- The vitamin D active ingredients mix with water and form structures called liposomes.
- The liposomes contain phospholipid bilayers of molecules and many of these surround the vitamin D to help protect and transport the nutrient.
- The vitamin D is incorporated into the fat molecules of the phospholipid-liposome bilayers.
- Because the liposome bilayers coating the vitamin D nutrient are similar to the cell walls themselves, they help provide easy access across your gut membrane into your bloodstream.
- Once the liposomes are absorbed from your GI tract into your bloodstream, they are able to penetrate more rapidly into the target tissues and cells where they are needed.
3. Vitamin D Dosage
How Much Vitamin D Should You Take per Day?
The RDI for Vitamin D is as follows (nih.gov):
400 IU (10 mcg): infants, 0–12 months
600 IU (15 mcg): children and adults, 1–70 years old
800 IU (20 mcg): older adults and pregnant or breastfeeding women
According to the U.S. National Academy of Medicine, the safe upper limit is 4,000 IU (100 mcg) per day (nih.gov).
To maintain healthy levels, only 400 to 800 IU (15 to 20 mcg) of vitamin D is required daily, but, to boost low levels, higher doses, such as 2,000 IU daily, are used and are generally safe.
However, many believe that the recommended intake is far too low and that people need much more to reach optimal blood levels (Trusted Source).
A group of researchers from the US, UK, Netherlands and New Zealand, said that the RDA of vitamin D should be increased to 2,000 IU and vitamin C to 200 mg in their review published in Nutrients 2020.
However, don’t consume more than 4,000 IU of vitamin D without your doctor’s permission. It exceeds the safe upper limits of intake and is not linked to more health benefits (Trusted Source).
4. Benefits of Vitamin D
Vitamin D is important to the body in many ways. It plays a significant role in optimizing health. Scientists are still discovering the many ways in which your body uses vitamin D for regulation and modulation.It helps the body absorb calcium from food and supplements. Muscles need it to move, for example, nerves need it to carry messages between the brain and every body part, and the immune system needs vitamin D to fight off invading bacteria and viruses. Together with calcium, vitamin D also helps protect older adults from osteoporosis. Vitamin D is found in cells throughout the body.
We have compiled and organised salient research in this article, on well over 20 health conditions (including COVID-19) that may be benefited from the use of vitamin D.
Vitamin D Benefits for Immune System
i. Vitamin D and Autoimmune Diseases
Vitamin D’s involvement in inflammation and both acquired and innate immune responses may explain why it appears to beneficial for preventing autoimmune diseases. Vitamin D receptors are present in nearly all cells of the human immune system, including monocytes/macrophages, T cells, B cells, natural killer cells and dendritic cells.
Because immune cells in autoimmune diseases like psoriasis respond to Vitamin D’s ameliorative effects , supplementing Vitamin D-deficient people with autoimmune disease may have benefits beyond bone and calcium homeostasis. (Source)
ii. Vitamin D and Infections
Vitamin D has multiple actions on the immune system, including enhancing the production of antimicrobial peptides by immune cells, reducing damaging proinflammatory cytokines and promoting the expression of anti-inflammatory cytokines.
Vitamin D deficiency affects the body’s susceptibility to infection and has been associated with influenza, hepatitis C, human immunodeficiency virus (HIV) and other viral diseases [Source].
According to Dr. Roger Seheult, Vitamin D..
- Stimulates “the innate immune response, which provides frontline protection against infectious agents”
- Increases expression of antimicrobial peptides in your monocytes and neutrophils
- Enhances expression of an antimicrobial peptide called human cathelicidin, “which is of specific importance in host defenses against respiratory tract pathogens”
iii. Vitamin D and Mortality
Vitamin D may also improve mortality. Some studies suggest that vitamin D reduces people’s risk of dying during the study periods, indicating that it may help you live longer (Source, Source).
iv. Vitamin D and Cancer - Studies
Vitamin D may help prevent cancer. One study noted that 1,100 IU per day — alongside calcium — reduced cancer risk by 60% (Source, Source).
A Harvard research study, published in the JAMA Network Open medical journal, overturns the initial findings of a study of 25,000 people published in 2018.
Initially researchers believed there was no benefit from taking vitamin D, as they detected no reduced incidence of cancer diagnoses overall. But they were puzzled because cancer deaths went down among those taking the supplements.
A secondary analysis, published last night, found this anomaly can be explained by the fact that vitamin D seems to stop metastatic cancers - those aggressive types which spread to other parts of the body.
Researcher Dr Paulette Chandler, a primary care physician and epidemiologist at Harvard's Brigham And Women's Hospital in Boston, said: 'Vitamin D is a supplement that's readily available, cheap and has been used and studied for decades.'
'Our findings, especially the strong risk reduction seen in individuals with normal weight, provide new information about the relationship between vitamin D and advanced cancer.'
Like Harvard's, most research on vitamin D and cancer shows a link between people who get enough of the vitamin and lower rates of the disease, less aggressive cancers and lower risks of dying from the disease.
In lab studies, pitting vitamin D against cancer cells showed that it can reduce their growth and keep them from multiplying and spreading. This may have to do with the role vitamin D plays in the life cycle of cells, and killing off unhealthy ones - but scientists are still studying whether what they've seen in the confines of a petri dish is true in the human body as well.
Vitamin D Benefits for Skin
i. Vitamin D for Dry or Itchy Skin
Severe dryness of the skin or Ichty can be an indicator of Vitamin D deficiency. Getting enough Vitamin D can improve symptoms of skin disorders that cause dry, itchy skin.ii. Vitamin D and Psoriasis
Oral Vitamin D supplementation is an important supplementary therapeutic choice for psoriatic patients. Vitamin D supplementation may also be crucial in preventing psoriasis-related comorbidities, hypertension and metabolic syndromes.iii. Vitamin D and Vitiligo
According to one study, high-dose Vitamin D therapy may be both safe and beneficial in the treatment of vitiligo. Sixteen vitiligo patients with low Vitamin D status were given 35,000 IU per day for six months, along with a dairy and calcium-rich food limitation and minimum hydration of 2.5 L per day. And the outcome, fourteen of them had repigmentation ranging from 25 to 75%.It’s still uncertain if high-dose supplementation provides any benefits for long-term patients with vitiligo.
iv. Vitamin D and Atopic Dermatitis
Vitamin D may play a role in improving the symptoms of Atopic Dermatitis. The findings of this study imply that Vitamin D supplementation may help reduce the severity of atopic dermatitis and can be considered as safe and manageable treatment option. However, this conclusion still needs larger-scale studies over a longer duration of treatment.v. Vitamin D Benefits For Acne
Acne is a common and complex skin disorder that can be stressful for many patients due to its chronicity. Although acne is caused by a number of factors, but chronic inflammation is an important mechanism.
According to a study, Vitamin D has an immune regulatory function in sebocytes, implying that Vitamin D may have anti-inflammatory properties in acne patients.
According to a study, Vitamin D has an immune regulatory function in sebocytes, implying that Vitamin D may have anti-inflammatory properties in acne patients.
Vitamin D Benefits For Women
If a woman is Vitamin D deficient during pregnancy, it may impact the bone health of her baby. Pregnant women who had a Vitamin D deficiency were more prone to preterm labor, premature birth or developing infections. They are also more likely to develop life-threatening high blood pressure (preeclampsia) and are also more likely to require a Cesarean section.
ii. Does Vitamin D Raise Estrogen Levels?
Yes, the Vitamin D levels in a woman’s body has a positive correlation with a woman’s estrogen levels. Those with higher levels of Vitamin D in their bodies tend to have higher levels of estrogen.
In fact, a deficiency in Vitamin D can lead to lower estrogen levels. This may lead to depression, hot flashes and mood swings.
i. Does Vitamin D Help Balance Hormones?
Yes. This is because Vitamin D is a hormone that communicates with other hormones. Thus, having sufficient Vitamin D2 and D3 can help ease and prevent hormonal fluctuations.ii. Does Vitamin D Raise Estrogen Levels?
Yes, the Vitamin D levels in a woman’s body has a positive correlation with a woman’s estrogen levels. Those with higher levels of Vitamin D in their bodies tend to have higher levels of estrogen.In fact, a deficiency in Vitamin D can lead to lower estrogen levels. This may lead to depression, hot flashes and mood swings.
Vitamin D Benefits for Men
Vitamin D is essential for muscle development as it is involved in the development of skeletal muscle. Vitamin D also plays an essential role in men’s sexual function and testosterone levels. Healthy levels of vitamin D may also benefit sexual health by mitigating the risk of cardiovascular disease.
i. Is Vitamin D Good For Testosterone?
Yes, Vitamin D may boost testosterone levels and also improve sperm quality.Vitamin D Benefits for Brain Health
i. Is Vitamin D Good For Depression?
It’s believed that vitamin D regulates more than 200 different genes by binding to vitamin D receptors that are responsible for driving a number of biological processes.Studies have shown that vitamin D deficiency is linked to even mild depression, and evidence suggests vitamin D deficiency may be a significant driver of the rise we see in both mood and mental disorders such as psychotic and obsessive-compulsive disorders.
This study suggests that adolescents with low levels of vitamin D had improved depressive symptoms ater vitamin D supplementation.
ii. How Much Vitamin D Should I Take For Depression ?
To know if you need high or low dosage, you’ll need to get a blood test. A result of 30 nmol/L (nanomoles per liter) or under is too low, and anything over 125 nmol/L is too high. Aim for 50 nmol/L or slightly above, according to the National Institutes of Health Office of Dietary Supplements (ODS).iii. Benefits of Vitamin D for Anxiety
Significantly lower levels of calcidiol were found in men and women with depression as well as in age matched patients with anxiety disorders. (Source)
A study found that taking Vitamin D supplements improved both depression and anxiety in women with type 2 diabetes.
The link between anxiety and Vitamin D still inconsistent, therefore further research is needed to fully understand the connection.
A study found that taking Vitamin D supplements improved both depression and anxiety in women with type 2 diabetes.
The link between anxiety and Vitamin D still inconsistent, therefore further research is needed to fully understand the connection.
Vitamin D Benefits for Weight Loss
i. Does Vitamin D Affect Metabolism?
Vitamin D is involved in the regulation of metabolic processes and development. This includes nerve conduction, normal mineralization of bone, muscle contraction, and general cellular function throughout the body. Vitamin D supplementation can increase physical strength in both upper and lower limbs (Trusted Source).ii. Does Vitamin D Help Lose Belly Fat?
Yes, Vitamin D can help trigger weight loss primarily in the belly. This is because Vitamin D and Calcium may work synergistically to reduce the production of cortisol, which is a stress hormone that causes you to store belly fat.iii. Vitamin D and Diabetes
Vitamin D reduces the risk of type 1 diabetes. One study in infants linked 2,000 IU of vitamin D per day to a 78% reduced risk of type 1 diabetes (Trusted Source).
Vitamin D Benefits for the Digestive System
An analysis of five studies examined the link between vitamin D blood levels and colorectal cancer (Trusted Source).
Scientists found that people with the highest blood levels of vitamin D (over 33 ng/ml or 82.4 nmol/l) had a 50% lower risk of colorectal cancer than people with the lowest levels of vitamin D (less than 12 ng/ml or 30 nmol/l).
Scientists found that people with the highest blood levels of vitamin D (over 33 ng/ml or 82.4 nmol/l) had a 50% lower risk of colorectal cancer than people with the lowest levels of vitamin D (less than 12 ng/ml or 30 nmol/l).
Vitamin D Benefits for the Heart
Studies (2017) have highlighted the importance of vitamin D for the prevention and treatment of heart disease, showing it plays a vital role in protecting and repairing damage to your endothelium. The findings also suggest vitamin D3:
- Helps trigger production of nitric oxide — a molecule known to play an important signaling role in controlling blood flow and preventing blood clot formation in your blood vessels
- Significantly reduces oxidative stress in your vascular system, which is important to help prevent the development and/or progression of cardiovascular disease
According to vitamin D researcher Dr. Michael Holick, author of “The Vitamin D Solution: A Three-Step Strategy to Cure Our Most Common Health Problem,” vitamin D deficiency — defined as a level below 20 ng/mL — can raise your risk of heart attack by 50%.
i. Research
An analysis of seventeen studies with over 300,000 people looked at the link between vitamin D intake and heart disease. Scientists found that taking 1,000 IU (25 mcg) of vitamin D daily reduced heart disease risk by 10% (Trusted Source).
Vitamin D has also been shown to have an anticoagulant effect. A decrease in 25-hydroxyvitamin D [25(OH)D] concentration has also been associated with an increased risk of venous thromboembolism (PubMed).
A Norwegian study published in the Journal of Clinical Endocrinology and Metabolism found “a normal intake of vitamin D” significantly reduces your risk of death if you have cardiovascular disease."
About 4,000 patients diagnosed with stable angina pectoris (chest pain caused by coronary heart disease) were followed for 12 years. The average age at the outset of the study was 62. Overall, those with vitamin D blood levels between 16.8 and 40 ng/mL (42 to 100 nmol/L) had the lowest mortality risk.
Vitamin D Benefits for Sleep
Several studies have found a link between lack of sleep, sleep disorders and vitamin D deficiency.
In 2012, Dr. Stasha Gominak, featured in the interview below, published a study in which she and her colleague used a two-year uncontrolled trial to evaluate the effect vitamin D supplementation had on neurological complaints and abnormal sleep patterns.
They engaged 1,500 people, in whom they maintained a narrow range of 25(OH)D levels between 60 nanograms per milliliter (ng/mL) and 80 ng/mL. These patients showed improvement in their sleep patterns and neurological symptoms.
Later studies by other teams of researchers found similar results. One paper published in 2014 suggested that recent reports of vitamin D deficiency may increase symptoms of airway muscle myopathy, chronic rhinitis and/or adenotonsillar hypertrophy, which may lead to obstructive sleep apnea.
One study in 2015 showed low levels of serum 25(OH)D in older men decrease sleep duration and efficiency, and a systematic review published in 2018 found vitamin D deficiency was linked to a higher risk of sleep disorders.
Also in 2018, a team of researchers evaluated vitamin D receptor genetic polymorphic variations and the impact serum concentration had on the susceptibility for obstructive sleep apnea syndrome. They found that one polymorphism explained 14.5% of the variability in serum concentration and was associated with excessive daytime sleepiness.
Finally, in late 2020, a paper published in Current Pharmaceutical Design sought to explore the role vitamin D plays in sleep regulation and the impact deficiency may have on sleep disorders. In a review of clinical trials and correlation studies they found vitamin D receptors and enzymes control activation expressed in the brain areas involved in sleep regulation. The team wrote:
“Furthermore, vitamin D can affect sleep indirectly through non-specific pain disorders, correlated with alterations in sleep quality, such as restless legs syndrome and obstructive sleep apnea syndrome.”
Vitamin D Benefits for Bone Health
Vitamin D is primarily known for helping to regulate calcium and phosphate, minerals that are key to developing and maintaining healthy bones, teeth and muscles. It does partly this by promoting the absorption of calcium and phosphorus from your gut (Source).
Vitamin D also helps your body absorb calcium from the food you eat. In fact, this is one of its most important roles.
Vitamin D reduces the risk of osteoporosis, falls, and fractures. Higher doses of vitamin D can help prevent osteoporosis, falls, and fractures in older adults (Source).
5. Vitamin D Foods
a. What Is The Best Way To Take Vitamin D?
Vitamin D is a fat-soluble vitamin, which means it does not dissolve in water and is best absorbed in the bloodstream when consumed with high-fat meals. That’s why the best way to take vitamin D supplement is with food to maximize absorption.According to one study in 17 people, taking vitamin D with the largest meal of the day increased vitamin D blood levels by about 50% after just 2–3 months (NIH).
In another study in 50 older adults, consuming vitamin D alongside a fat-heavy meal increased vitamin D blood levels by 32% after 12 hours compared to a fat-free meal (NIH).
Avocados, nuts, seeds, full-fat dairy products and eggs are nutritious sources of fat that help boost your vitamin D absorption.
b. Foods That Are High In Vitamin D
| Food | Amount | % RDI |
| Cod liver oil, 1 tablespoon (15 ml) | 1,360 IU / 34 mcg | 227% |
| Salmon, cooked, 3 ounces (85 grams) | 447 IU / 11 mcg | 75% |
| Tuna, canned in water, 3 ounces (85 grams) | 154 IU / 4 mcg | 26% |
| Beef liver, cooked, 3 ounces (85 grams) | 42 IU / 1 mcg | 7% |
| 1 large whole egg (D is found in yolk) | 41 IU / 1 mcg | 7% |
| 1 sardine, canned in oil, drained | 23 IU / 0.6 mcg | 4% |
Although fatty fish like salmon, mackerel, swordfish, trout, tuna, and sardines are decent sources, you would have to eat them almost every day to get enough.
The only excellent dietary source of vitamin D is fish liver oil — such as cod liver oil — which contains upwards of two times the Reference Daily Intake (RDI) in a single tablespoon (15 ml).
Keep in mind that dairy products and cereals are often fortified with vitamin D (NIH).
The only excellent dietary source of vitamin D is fish liver oil — such as cod liver oil — which contains upwards of two times the Reference Daily Intake (RDI) in a single tablespoon (15 ml).
Keep in mind that dairy products and cereals are often fortified with vitamin D (NIH).
c. Vitamin D Fruits
Orange juice - A cup (237 ml) of fortified orange juice contains up to 100 IU of Vitamin D.d. Vitamin D Vegetables
Mushrooms - Mushrooms are a good source of Vitamin D2. Mushrooms produce Vitamin D2 when exposed to UV light.6. Vitamin D and Other Supplements
When supplementing, also remember to take synergistic effects with other nutrients into account. If you take high-dose vitamin D, you may also need to increase your intake of Vitamin K2 and Magnesium.
These nutrients all work in tandem, and rely on sufficient amounts of each to work optimally.
a. Vitamin D3 and Vitamin K2
Vitamin K2 supplements have been proven to be more effective than vitamin K1. That's why most of the top vitamin D supplement brands do combine their vitamin D3 with K2.
Low levels of vitamin D and vitamin K have also been linked to high blood pressure (Source).
i. Bone Health
Half of adults over 50 years of age have low bone mass. Bone health is a real concern as we get older. Vitamin D ensures that your blood levels of calcium are high enough to meet your body’s demands.
However, vitamin D does not fully control where the calcium in your body ends up. That’s where vitamin K steps in. The pairing of vitamin D3 and K2 seems to improve bone health across the board.
Excessive vitamin D in combination with lack of vitamin K2 may cause overabsorption of calcium, which in turn may result in calcium deposits in your heart and kidneys. Part of the explanation for these adverse side effects is that vitamin K2 keeps calcium in its appropriate place — in your teeth and bones and out of soft tissues and arteries.
While the optimal ratios between vitamin D and vitamin K2 have yet to be established, taking somewhere between 100 to 200 micrograms (mcg) of K2 is beneficial. Telltale signs of vitamin K2 insufficiency include osteoporosis, heart disease and diabetes. You’re also more likely to be deficient if you rarely eat vitamin K2-rich foods (see listing below).
ii. Research
A groundbreaking 2017 review compiled over 80 studies that show vitamin D3 and K2 together might be greater than the sum of their parts, when it comes to bone health.
This is likely because vitamin D gets the calcium into the blood, then vitamin K tells the calcium where it is most needed.
Taking vitamin D3 and K2 together actually promotes new bone growth. In 2019, researchers observed that vitamin D3 and K2 worked in tandem to form new osteoblasts, the cells that secrete osteocalcin, which is a biomarker for new bone growth.
iii. Vitamin K2 Foods
Grass fed organic animal products such as eggs and butter, fermented foods such as natto, goose liver pâté and vitamin K2-rich cheeses such as Brie and Gouda.
b. Vitamin D and Magnesium
Magnesium, the fourth most abundant mineral in your body, is a component necessary for the activation of vitamin D, and without sufficient amounts of it, your body cannot properly utilize the vitamin D you’re taking. (Source, Source, Source, Source)
This may actually help explain why many need rather high doses of vitamin D to optimize their levels — it could be that they simply have insufficient amounts of magnesium in their system to activate the vitamin D.
As noted by coauthor Mohammed Razzaque, professor of pathology at Lake Erie College of Osteopathic Medicine in Pennsylvania:
"People are taking vitamin D supplements but don't realize how it gets metabolized. Without magnesium, vitamin D is not really useful. By consuming an optimal amount of magnesium, one may be able to lower the risks of vitamin D deficiency, and reduce the dependency on vitamin D supplements.”
As reported in the press release by the American Osteopathic Association:
“… [C]onsumption of vitamin D supplements can increase a person's calcium and phosphate levels even if they remain vitamin D deficient. The problem is people may suffer from vascular calcification if their magnesium levels aren't high enough to prevent the complication. Patients with optimum magnesium levels require less vitamin D supplementation to achieve sufficient vitamin D levels …
Deficiency in either of these nutrients is reported to be associated with various disorders, including skeletal deformities, cardiovascular diseases, and metabolic syndrome. While the recommended daily allowance for magnesium is 420 mg for males and 320 mg for females, the standard diet in the United States contains only about 50 percent of that amount.
As much as half of the total population is estimated to be consuming a magnesium-deficient diet.”
Furthermore, higher magnesium intake helps reduce your risk of vitamin D deficiency. As noted in one 2013 study:
“Magnesium plays an essential role in the synthesis and metabolism of vitamin D and magnesium supplementation substantially reversed the resistance to vitamin D treatment in patients with magnesium-dependent vitamin-D-resistant rickets … High intake of total, dietary or supplemental magnesium was independently associated with significantly reduced risks of vitamin D deficiency and insufficiency respectively.
Intake of magnesium significantly interacted with intake of vitamin D in relation to risk of both vitamin D deficiency and insufficiency. Additionally, the inverse association between total magnesium intake and vitamin D insufficiency primarily appeared among populations at high risk of vitamin D insufficiency.
Furthermore, the associations of serum 25(OH)D with mortality, particularly due to cardiovascular disease and colorectal cancer, were modified by magnesium intake, and the inverse associations were primarily present among those with magnesium intake above the median. Our preliminary findings indicate it is possible that magnesium intake alone or its interaction with vitamin D intake may contribute to vitamin D status.”
i. Vitamin D and Magnesium for Covid-19
While vitamin D and magnesium are important for overall health year-round, they may be of particular importance right now, as we're still dealing with the COVID-19 pandemic in many areas of the world, and a second wave is expected in the fall.
A review by Dinicolantonio et al (Mo Med Feb 2021) also suggested vitamin D and magnesium deficiency as a potential cause of cytokine storm in COVID-19 patients and recommended that vitamin D and magnesium supplementation to be considered.
ii. Magnesium Foods
Almonds and cashews, bananas, broccoli and Brussels sprouts, brown rice, free-range pastured egg yolk, flaxseed, grass fed raw milk, mushrooms, pumpkin seeds, sesame seeds, sunflower seeds and leafy green vegetables, especially spinach, Swiss chard, turnip greens, beet greens, collard greens, kale, Bok Choy and romaine lettuce
c. Vitamin D3, Vitamin K2 and Magnesium
Vascular calcification is a side effect of low magnesium, so when taking vitamin D3, you need both vitamin K2 and magnesium to make sure everything is working properly. Magnesium and vitamin K2 also complement each other, as magnesium helps lower blood pressure, which is an important component of heart disease.
According to research by GrassrootsHealth, "combined intake of both supplemental magnesium and vitamin K2 has a greater effect on vitamin D levels than either individually,".
This research also mentions that "those taking both supplemental magnesium and vitamin K2 have a higher vitamin D level for any given vitamin D intake amount than those taking either supplemental magnesium or vitamin K2 or neither."
Data from nearly 3,000 individuals reveal you need 244% more oral vitamin D if you're not also taking magnesium and vitamin K2. As reported by GrassrootsHealth:
"… 244% more supplemental vitamin D was needed for 50% of the population to achieve 40 ng/ml (100 nmol/L) for those not taking supplemental magnesium or vitamin K2 compared to those who usually took both supplemental magnesium and vitamin K2."
What this means in practical terms is that if you take all three supplements in combination, you need far less oral vitamin D in order to achieve a healthy vitamin D level.
d. Vitamin D and Melatonin
Vitamin D is involved in the pathways that produce melatonin in the pineal gland. Meanwhile, melatonin is involved with dictating our circadian rhythm (Source, Source).
An evaluation of clinical trials and correlation studies have shown that “Vitamin D has both a direct and indirect role in the regulation of sleep.”
Melatonin, the hormone secreted by your pineal gland located near the center of the brain, is crucial for the regulation of your sleep cycle. With enough exposure to bright light during the daytime, the gland starts secreting melatonin during the evening darkness.
As this amount increases the body prepares for sleep. When you stay up past dark using artificial light, especially light emitted by electronic devices, it inhibits melatonin production. Ideally, you would stop using electronics at least an hour or two before bedtime. This helps to raise your melatonin production and maintain a steady circadian rhythm.
e. Vitamin D and Omega 3
i. Synergistic Effects against Autoimmune Diseases
Researchers from Brigham and Women’s Hospital, Harvard Medical School, used data from the vitamin D and omega-3 trial (VITAL), which involved 25,871 participants aged 50 (men) or 55 (women) and older, to investigate whether vitamin D and omega-3 fats from marine sources reduce the risk of autoimmune disease.
Participants took vitamin D3 (2,000 IU), omega-3 fats (1,000 milligrams) or a placebo daily and were followed for more than five years. They self-reported all autoimmune diseases that were diagnosed during the study period, and those taking vitamin D and/or omega-3s had a lower risk.
“Vitamin D supplementation for five years, with or without omega-3 fatty acids, reduced autoimmune disease by 22%, while omega-3 fatty acid supplementation with or without vitamin D reduced the autoimmune disease rate by 15% (not statistically significant),” the researchers wrote.
For those taking both vitamin D and omega-3 fats, the risk of autoimmune disease decreased by about 30%. Further, when participants took vitamin D for at least two years, their risk of autoimmune disease decreased even more — by 39%.
7. Vitamin D Deficiency
According to Dr John Campbell:
- Deficiency: Less than 20 ng/ml (50 nmol/L)
- Insufficiency: 21 - 29 ng/ml (52 - 72 nmol/L)
- Sufficiency: More than 30 ng/ml (75 nmol/L)
In the United States, 41.6% of the total population is deficient, although minorities fare worse — 82.1% and 69.2% of blacks and Hispanics are deficient, respectively (Trusted Source).
An analysis of data from the 2015–2016 National Health and Nutrition Examination Survey (NHANES) found that average daily vitamin D intakes from foods and beverages were 5.1 mcg (204 IU) in men, 4.2 mcg (168 IU) in women, and 4.9 mcg (196 IU) in children aged 2–19 years (NHANES).
A recent publication (Aug 2020) from the International Journal of Infectious Diseases, highlighted that the majority of the Western population is deficient in Vitamin D. According to the author, the immunoregulating function of Vitamin D is promising and might decrease the global epidemic mortality.
a. Symptoms of Vitamin D Deficiency
Vitamin D deficiency is often a silent epidemic. The symptoms are usually subtle and may take years or decades to surface.
A blood test is the best way to determine your vitamin D levels, but here are some vitamin D deficiency symptoms that may indicate your levels are low:
- Aching muscles
- Painful bones
- Fatigue
- Reduced muscle performance
- Brain health
- Poor sleep
- Sweaty head
- Hair loss
- Slow-healing wounds
- Dizziness
- Heart problems
- Excess weight
- Recurring infections
- Reduced cognitive function
b. Risks of Vitamin D Deficiency
Well-known symptom of Vitamin D deficiency is rickets, a bone disease common in children in developing countries. Rickets has been mostly eliminated from Western countries because of the fortification of some foods with Vitamin D (Trusted Source).
Deficiency is also linked to osteoporosis, reduced mineral density, and increased risk of falls and fractures in older adults (Source).
One study showed that 96% of people who had experienced heart attacks were low in Vitamin D (Trusted Source).
What’s more, studies indicate that people with low Vitamin D levels have a much greater risk of heart disease, diabetes (types 1 and 2), cancer, dementia, and autoimmune diseases like multiple sclerosis (Trusted Source).
Finally, Vitamin D deficiency is linked to a reduced life expectancy (Trusted Source, Trusted Source, Trusted Source).
That said, it’s unclear whether deficiency contributes to these diseases or whether people with low levels are just more likely to get them.
What’s more, studies indicate that people with low Vitamin D levels have a much greater risk of heart disease, diabetes (types 1 and 2), cancer, dementia, and autoimmune diseases like multiple sclerosis (Trusted Source).
Finally, Vitamin D deficiency is linked to a reduced life expectancy (Trusted Source, Trusted Source, Trusted Source).
That said, it’s unclear whether deficiency contributes to these diseases or whether people with low levels are just more likely to get them.
c. Risk Factors of Vitamin D Deficiency
Risk factors for vitamin D deficiency include..
i. It’s winter and you don’t live in the tropics or subtropics.
There simply isn’t enough, or even any UVB that reaches the ground in the winter if you are not in the tropics or subtropics, and exposure to UVB is how your body produces most of the vitamin D it requires naturally.
ii. You have darker skin.
Those with darker skin may need as much as 10 times more sun exposure to produce the same amount of vitamin D as a person with pale skin.
iii. You're 50 or older. (Trusted Source)
As you get older, your skin produces less vitamin D when exposed to the sun.
iv. You spend a lot of time indoors.
If you avoid the sun or just aren’t able to get outdoors regularly, your levels of vitamin D are likely to be lower.
v. You're overweight or obese (or have a higher muscle mass).
Vitamin D is a fat-soluble, hormone-like vitamin, so body fat can act like a sponge. A heavier person with more body fat or even those with more muscle mass may require a higher dose than a slimmer person.
vi. You have gut issues.
If you have a gastrointestinal condition that affects your ability to absorb fat you may have lower absorption of vitamin D.
vii. You’re achy or tired, or both.
The classic signs of a certain type of vitamin D deficiency can mimic conditions characterized by fatigue and achy bones.
viii. You sometimes feel blue.
Serotonin, the brain hormone associated with mood elevation, rises with exposure to bright light and falls with decreased sun exposure.
ix. You’re pregnant.
Pregnant women require higher amounts of vitamin D for their own pregnancy and delivery as well as the optimal health of their babies.
x. You notice unusual head sweating.
Surprisingly, one of the first signs of a vitamin D deficiency is a sweaty head.
8. Side Effects of Vitamin D
High doses of vitamin D can result in a condition called hypervitaminosis D. Hypervitaminosis is a rare but serious condition that could put you at risk for liver or kidney problems.
The main symptoms of toxicity include confusion, lack of concentration, drowsiness, depression, vomiting, abdominal pain, constipation, and high blood pressure (Trusted Source). Other side effects of Vitamin D include..
a. Elevated blood levels
Although a vitamin D level of 30 ng/ml (75 nmol/l) is typically considered adequate, the Vitamin D Council recommends maintaining levels of 40–80 ng/ml (100–200 nmol/l) and states that anything over 100 ng/ml (250 nmol/l) may be harmful (Trusted Source).While an increasing number of people are supplementing with vitamin D, it’s rare to find someone with very high blood levels of this vitamin.
One recent study looked at data from more than 20,000 people over a 10-year period. It found that only 37 people had levels above 100 ng/ml (250 nmol/l). Only one person had true toxicity, at 364 ng/ml (899 nmol/l) (Trusted Source).
In one case study, a woman had a level of 476 ng/ml (1,171 nmol/l) after taking a supplement that gave her 186,900 IU of vitamin D3 per day for two months.
This was a whopping 47 times the generally recommended safe upper limit of 4,000 IU per day. The woman was admitted to the hospital after she experienced fatigue, forgetfulness, nausea, vomiting, slurred speech, and other symptoms.
Although only extremely large doses can cause toxicity so rapidly, even strong supporters of these supplements recommend an upper limit of 10,000 IU per day (Trusted Source).
b. Elevated blood calcium levels
If vitamin D intake is excessive, blood calcium may reach levels that can cause unpleasant and potentially dangerous symptoms.Symptoms of hypercalcemia, or high blood calcium levels, include:
- digestive distress, such as vomiting, nausea, and
- stomach pain
- fatigue, dizziness, and confusion
- excessive thirst
- frequent urination
In one case study, an older man with dementia who received 50,000 IU of vitamin D daily for 6 months was repeatedly hospitalized with symptoms related to high calcium levels (Trusted Source).
In another, two men took improperly labeled vitamin D supplements, leading to blood calcium levels of 13.2–15 mg/dl (3.3–3.7 mmol/l). What’s more, it took a year for their levels to normalize after they stopped taking the supplements (Trusted Source).
c. Nausea, vomiting, and poor appetite
Many side effects of too much vitamin D are related to excessive calcium in the blood. These include nausea, vomiting, and poor appetite. However, these symptoms don’t occur in everyone with elevated calcium levels.One study followed 10 people who had developed excessive calcium levels after they had taken high-dose vitamin D to correct deficiency. Four of them experienced nausea and vomiting, and three of them had a loss of appetite (Trusted Source).
Similar responses to vitamin D megadoses have been reported in other studies. One woman experienced nausea and weight loss after taking a supplement that was found to contain 78 times more vitamin D than stated on the label (Trusted Source, Trusted Source).
Importantly, these symptoms occurred in response to extremely high doses of vitamin D3, which led to calcium levels greater than 12 mg/dl (3.0 mmol/l).
d. Stomach pain, constipation, or diarrhea
Stomach pain, constipation, and diarrhea are common digestive complaints that are often related to food intolerances or irritable bowel syndrome. However, they can also be a sign of elevated calcium levels caused by vitamin D intoxication (Trusted Source).These symptoms may occur in those receiving high doses of vitamin D to correct deficiency. As with other symptoms, response appears to be individualized even when vitamin D blood levels are similarly elevated.
In one case study, a boy developed stomach pain and constipation after taking improperly labeled vitamin D supplements, whereas his brother experienced elevated blood levels without any other symptoms (Trusted Source).
In another case study, an 18-month-old child who was given 50,000 IU of vitamin D3 for 3 months experienced diarrhea, stomach pain, and other symptoms. These symptoms resolved after the child stopped taking the supplements (Trusted Source).
In another case study, an 18-month-old child who was given 50,000 IU of vitamin D3 for 3 months experienced diarrhea, stomach pain, and other symptoms. These symptoms resolved after the child stopped taking the supplements (Trusted Source).
e. Bone loss
Too much vitamin D can be detrimental to bone health. Although many symptoms of excessive vitamin D are attributed to high blood calcium levels, some researchers suggest that megadoses may lead to low levels of vitamin K2 in the blood (Trusted Source).One of vitamin K2’s most important functions is to keep calcium in the bones and out of the blood. It’s believed that very high vitamin D levels may reduce vitamin K2 activity (Trusted Source, Trusted Source).
To protect against bone loss, avoid taking excessive vitamin D supplements and take a vitamin K2 supplement. You can also eat foods rich in vitamin K2, such as grass-fed dairy and meat.
A 3-year study published in the Aug. 27, 2019 issue of JAMA found that, compared with people who took moderate amounts of Vitamin D (400 IU), adults who took large amounts daily (4,000 IU) not only didn’t see additional gains in bone density, but in some cases ended up worse off.
f. Kidney failure
Excessive vitamin D intake frequently results in kidney injury.In one case study, a man was hospitalized for kidney failure, elevated blood calcium levels, and other symptoms that occurred after he received vitamin D injections prescribed by his doctor (Source).
Indeed, most studies have reported moderate-to-severe kidney injury in people who develop vitamin D toxicity (Trusted Source, Trusted Source, Trusted Source, Trusted Source, Trusted Source, Trusted Source).
In one study in 62 people who received excessively high-dose vitamin D injections, each person experienced kidney failure — whether they had healthy kidneys or existing kidney disease (Trusted Source). Kidney failure is treated with oral or intravenous hydration and medication.
9. How To Measure Vitamin D Levels
How Do You Know That Your Vitamin D Level is Adequate?
a. Vitamin D Test Kits
- Buy Vitamin D Test Kit
b. Grassroot Health's Vitamin D Calculator
To make sure your vitamin D level and immune system function are optimized, follow these three steps:
i. First, measure your vitamin D level — Once you know what your blood level is, you can assess the dose needed to maintain or improve your level. The easiest way to raise your level is by getting regular, safe sun exposure, but if you're very dark-skinned, you may need to spend about 1.5 hours a day in the sun to have any noticeable effect.
Those with very light skin may need only 15 minutes a day, which is far easier to achieve. Still, they too will typically struggle to maintain ideal levels during the winter. So, depending on your situation, you may need to use an oral vitamin D3 supplement. The next question then becomes, how much do you need?
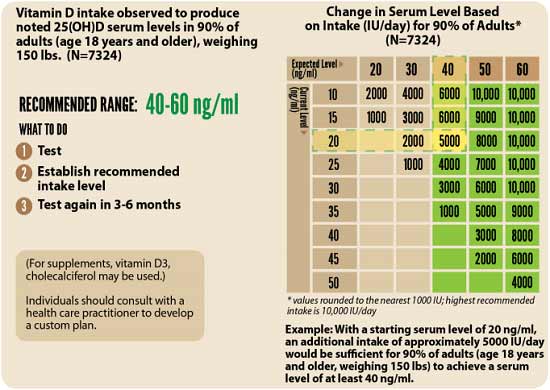
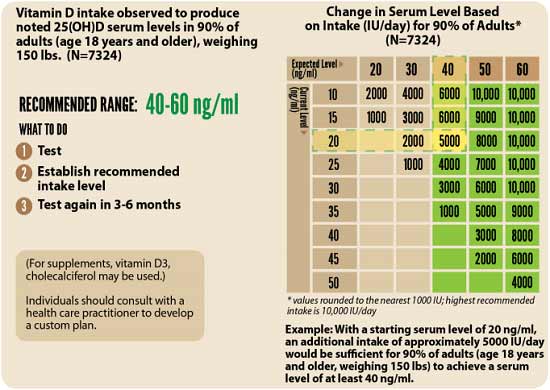
ii. Assess your individualized vitamin D dosage — To do that, you can either use the chart below, or use GrassrootsHealth's Vitamin D calculator. To convert ng/mL into the European measurement (nmol/L), simply multiply the ng/mL measurement by 2.5. To calculate how much vitamin D you may be getting from regular sun exposure in addition to your supplemental intake, consider using the DMinder app.
iii. Retest in three to six months — Lastly, you'll need to remeasure your vitamin D level in three to six months, to evaluate how your sun exposure and/or supplement dose is working for you.
c. Measuring Vitamin D Levels In Blood - Vitamin D Hydroxy Test
i. What is 25-hydroxy Vitamin D?
Vitamin D must go through several processes in your body before your body can use it. The first transformation occurs in the liver.Here, the liver converts vitamin D2 into 25-hydroxyvitamin D2 and vitamin D3 into 25-hydroxyvitamin D3. These two compounds are collectively known as calcifediol (also known as calcidiol).
Calcifediol is the main circulating form of vitamin D, and its blood levels reflect your body’s stores of this nutrient.
For this reason, your health care provider can estimate your vitamin D status by measuring your levels of calcifediol (Trusted Source).
However, vitamin D2 seems to yield less calcifediol than an equal amount of vitamin D3.
Most studies show that vitamin D3 is more effective than vitamin D2 at raising blood levels of calcifediol (Trusted Source, Trusted Source).
The test is also known as the 25-OH vitamin D test and the calcidiol 25-hydroxycholecalciferol test. It can be an important indicator of osteoporosis (bone weakness) and rickets (bone malformation).
Calcifediol is the main circulating form of vitamin D, and its blood levels reflect your body’s stores of this nutrient.
For this reason, your health care provider can estimate your vitamin D status by measuring your levels of calcifediol (Trusted Source).
However, vitamin D2 seems to yield less calcifediol than an equal amount of vitamin D3.
Most studies show that vitamin D3 is more effective than vitamin D2 at raising blood levels of calcifediol (Trusted Source, Trusted Source).
ii. What is the 25-hydroxy Vitamin D test?
The 25-hydroxy vitamin D test is the best way to monitor vitamin D levels. The amount of 25-hydroxyvitamin D in your blood is a good indication of how much vitamin D your body has. The test can determine if your vitamin D levels are too high or too low.The test is also known as the 25-OH vitamin D test and the calcidiol 25-hydroxycholecalciferol test. It can be an important indicator of osteoporosis (bone weakness) and rickets (bone malformation).
iii. What is the 25 Dihydroxy Vitamin D1 test?
There is another blood test for normal vitamin D levels, called Vitamin D 1,25 Dihydroxy level or 1,25(OH)(2)D.
The Vitamin D, 1,25 Dihydroxy level does not have a major change until normal Vitamin D levels drop to levels that are considered a VERY severe Vitamin D deficiency. Calcidiol is converted to calcitriol, or 1,25(OH)2D, mostly in your kidneys. This is the active, steroid-hormone form of vitamin D.
The Vitamin D, 1,25 Dihydroxy level does not have a major change until normal Vitamin D levels drop to levels that are considered a VERY severe Vitamin D deficiency. Calcidiol is converted to calcitriol, or 1,25(OH)2D, mostly in your kidneys. This is the active, steroid-hormone form of vitamin D.
Calcitriol interacts with the vitamin D receptor (VDR), which is found in almost every single cell in your body (Trusted Source, Trusted Source). When the active form of vitamin D binds to this receptor, it turns genes on or off, leading to changes in your cells. This is similar to how most other steroid hormones work (Trusted Source, Trusted Source).
1,25 dihydroxy-vitamin D or 1.25 Dihydroxy level has the normal values that are usually listed as 20-76 pg/ml.
Normal Vitamin D Lab Values for 1,25 Dihydroxy Vitamin D
Normal Vitamin D Lab Values for 1,25 Dihydroxy Vitamin D
- Adults in good health (age 20-50) : 17 - 53 pg/ml
- Children up to 12: ca. 40% higher values
- Pregnant women (8-42 week): ca. 60% higher values
- Persons older than 70: ca. 40% lower values
- The normal range is independent of the season.
Most considered the most potent form of vitamin D. It stimulates calcium absorption from our small intestines and bones (along with PTH) and increases reabsorption of calcium by the kidneys.
The level of serum 1,25-dihydroxy-vitamin D is not typically used to know vitamin D status. It has a short half-life of only 15 hours. It is regulated by parathyroid hormone, calcium, and phosphate. So a decrease will not be noted until vitamin D deficiency is severe.
iv. Why is a 25-hydroxy Vitamin D test done?
Your doctor may request a 25-hydroxy vitamin D test for several different reasons. It can help them figure out whether too much or too little vitamin D is causing bone weakness or other abnormalities. It can also monitor people who are at risk for having a vitamin D deficiency.Those who are at high risk of having low levels of vitamin D include:
- people who don’t get much exposure to the sun
- older adults
- people with obesity
- babies who are breastfed only (formula is usually fortified with vitamin D)
- people who have had gastric bypass surgery
- people who have a disease that affects the intestines and makes it difficult for the body to absorb nutrients, such as Crohn’s disease
v. How is the 25-hydroxy Vitamin D test performed?
The 25-hydroxy vitamin D test requires a common blood test. Your healthcare provider will draw blood from a vein in your arm using a needle. A quick finger prick will more than likely provide enough for a blood sample in children and infants.Your doctor will tell you not to eat anything for four to eight hours before the test.
vi. Evaluating the results of a 25-hydroxy Vitamin D test
Your doctor will help explain the results of your test and determine if you have a vitamin D deficiency.
According to the Office of Dietary Supplements (ODS), levels of vitamin D are measured by the 25-hydroxy level in nanomoles/liter (nmol/L) or nanograms/milliliter (ng/mL). The results can indicate the following:
- deficiency: less than 30 nmol/L (12 ng/mL)
- potential deficiency: between 30 nmol/L (12 ng/mL) and 50 nmol/L (20 ng/mL)
- normal levels: between 50 nmol/L (20 ng/mL) and 125 nmol/L (50 ng/mL)
- high levels: higher than 125 nmol/L (50 ng/mL)
Low blood levels of 25-hydroxy vitamin D usually mean one (or more) of the following:
- you aren’t eating a balanced, complete diet
- your intestines aren’t absorbing the vitamin properly
- you’re not spending enough time outside to absorb adequate vitamin D levels through sun exposure
vii. Risks of a 25-hydroxy Vitamin D test
10. Does Vitamin D Interact With Medications or Other Supplements?
Vitamin D supplements may interact with certain medications, such as:- Orlistat: This weight-loss drug, in combination with a reduced-fat diet, may reduce the absorption of vitamin D from food and supplements, leading to lower 25(OH)D levels.
- Statins: Cholesterol-lowering statin medications could be less effective with high vitamin D intake as both statins and vitamin D compete for the same metabolizing enzyme. High vitamin D intake, especially from supplements, might affect the potency of certain statins.
- Steroids: Corticosteroid medications, such as prednisone, prescribed for inflammation, can decrease calcium absorption and impair vitamin D metabolism.
- Thiazide diuretics: When combined with vitamin D supplements that increase intestinal calcium absorption, these diuretics may lead to markedly high calcium levels. This is particularly relevant for older adults and individuals with compromised renal function or hyperparathyroidism.
- Calcipotriene: Combining vitamin D supplements with calcipotriene, a psoriasis medication applied topically, may elevate blood calcium levels to a dangerous extent.
- Calcium channel blockers: Vitamin D may counteract the effects of calcium channel blockers, medications prescribed for high blood pressure and heart conditions. Examples of calcium channel blockers include nifedipine, verapamil, nicardipine, diltiazem, and amlodipine.
- Digoxin: Even low levels of digoxin, a medication for irregular heart rhythms, can become toxic if calcium levels are raised too high by taking vitamin D supplements.
- Estrogen medications: Hormone replacement therapy with estrogen can elevate vitamin D levels, potentially benefiting calcium and bone strength. Combining vitamin D supplements with estrogen replacement therapy may enhance bone mass, but this effect may vary if progesterone is also taken.
- Isoniazid: Isoniazid, a drug used in tuberculosis treatment, could potentially lower vitamin D levels in the bloodstream.
- Antacids: Long-term use of certain antacids used to treat heartburn and indigestion might impact the levels, metabolism, and accessibility of vitamin D.
- Anti-seizure medications: Anti-seizure drugs, including phenobarbital, phenytoin, primidone, and valproic acid, can reduce vitamin D levels.
- Bile acid sequestrants: These drugs are prescribed to lower cholesterol, including cholestyramine and colestipol, and can reduce vitamin D levels.
- Mineral oil: Mineral oil disrupts the absorption of vitamin D.
- Anti-HIV drugs: Certain anti-HIV drugs, such as efavirenz and AZT, may lower vitamin D levels, while darunavir exposure seems to increase vitamin D levels.
- Antifungal agents: Antifungal agents such as clotrimazole and ketoconazole can also decrease vitamin D levels.
- Medicinal herbs: St. John’s wort or its extracts, such as hypericin and hyperforin, may reduce vitamin D levels.
11. Online Shopping Guide
1. Nature Made Vitamin D3 2000iu - Vitamin D Supplement for Immune Support
2. Horbäach Vitamin D3 2000iu Gummies - Vitamin D Supplement for Acne
3. Bronson Vitamin D3 2,000iu - Vitamin D Supplement for Skin .
4. Mary Ruth's Vitamin D3 + B12 Gummies - Vitamin D Supplement for Women
5. Life Extension Vitamin D3 5000 IU - Vitamin D Supplement for Men
6. NOW Vitamin D3 5000iu - Vitamin D Supplement for Anxiety
7. NOW Supplements, Vitamin D-3 & K-2, 1,000 IU/45 mcg - Vitamin D Supplement for Weight Loss
9. Bronson Vitamin D3 Plus K2 - Vitamin D3 K2 Supplement
10. Mary Ruth's Vegan Organic Vitamin D3 + K2 - Liquid Vitamin D3 with K2
11. Zahler Junior D3 Chewable 1000 IU - Vitamin D Supplement for Kids
12. Upnourish Liposomal Vitamin D3 K2 MK7 : 5000 IU / 100 mcg - Liposomal Vitamin D3 K2
13. Upnourish Liposomal Vitamin D3 5000 IU Softgels - Vitamin D Liposomal
14. NOW Supplements, Vitamin D-3 & K-2 Liposomal Spray 1,000 IU/100 mcg - Liposomal Vitamin D3 Spray
.png)
.png)


.png)
.jpg)



Comments