Best Ways to Prevent Cancer: Unveiling the Science Behind Cancer, Diet and Supplements (300+ Studies Analyzed)
We can recall notable figures like Steve Jobs, Chadwick Boseman (Black Panther), Robin Gibb (Bee Gees), Donna Summer, Farrah Fawcett, Eartha Kitt, Peter Jennings, Paul Newman, Patrick Swayze, Sydney Pollack, Michael Crichton, Bob Denver, Ted Kennedy, Jerry Orbach, Anne Bancroft, William Rehnquist, and Tony Snow, among others. What unites them? They all succumbed to 'cancer.'
Many of these individuals had access to the finest medical care available worldwide. So, what is the missing link here? Does cancer still elude our understanding? Is it preventable?
Can our dietary choices impact our susceptibility to cancer? Which foods can reduce the risk, and which might heighten it? How do vitamin and mineral supplements come into play? Do they mitigate or potentially increase the risk of cancer? Admittedly, numerous guides exist on this subject, but most tend to be product-centric, biased, and lack the most current and evidence-based information.
In this Article:
- What is Cancer?
- Diet and Cancer Prevention
- Cancer Fighting Foods
- Berries and Fruits
- Broccoli
- Turmeric (Curcumin)
- Tomato (Lycopene)
- Carrots
- Beans
- Nuts
- Olive Oil
- Soy
- Cancer and supplements
- Vitamin D3, K2 and Magnesium
- Curcumin (Turmeric)
- Omega-3 Fatty Acids
- EGCG (Green tea)
- Allicin (Garlic)
- Quercetin
- Molecular Hydrogen
- Melatonin
- Resveratrol
- Vitamin C and B6
- Probiotics
- Don't use tobacco
- Maintain a healthy weight and be physically active
- Avoid risky behaviors
- Protect yourself from the sun
- Get regular medical care and Health Screening
- Avoid unnecessary exposure to radiation.
- Sleep Quality and Reduce Stress
- Avoid exposure to environmental toxins and infections that contribute to cancer
What is Cancer?
Cancer is the second leading cause of death in the United States, behind only heart disease. For most Americans who do not use tobacco, the most important cancer risk factors that can be changed are body weight, diet, and physical activity. At least 18% of all cancers diagnosed in the US are related to excess body weight, physical inactivity, excess alcohol consumption, and/or poor nutrition, and thus could be prevented.Genetic changes that cause cancer can be inherited from our parents. That said, environmental factors could contribute up to 95% of cancers. They can also arise during a person’s lifetime as a result of errors that occur as cells divide or because of damage to DNA caused by certain environmental exposures. Cancer-causing environmental exposures include substances, such as the chemicals in tobacco smoke, and radiation, such as ultraviolet rays from the sun.
There are many types of cancer treatment. The types of treatment that you receive will depend on the type of cancer you have and how advanced it is. Surgery, radiation, and chemotherapy are the standard types of treatment for cancer.
Diet and Cancer Prevention
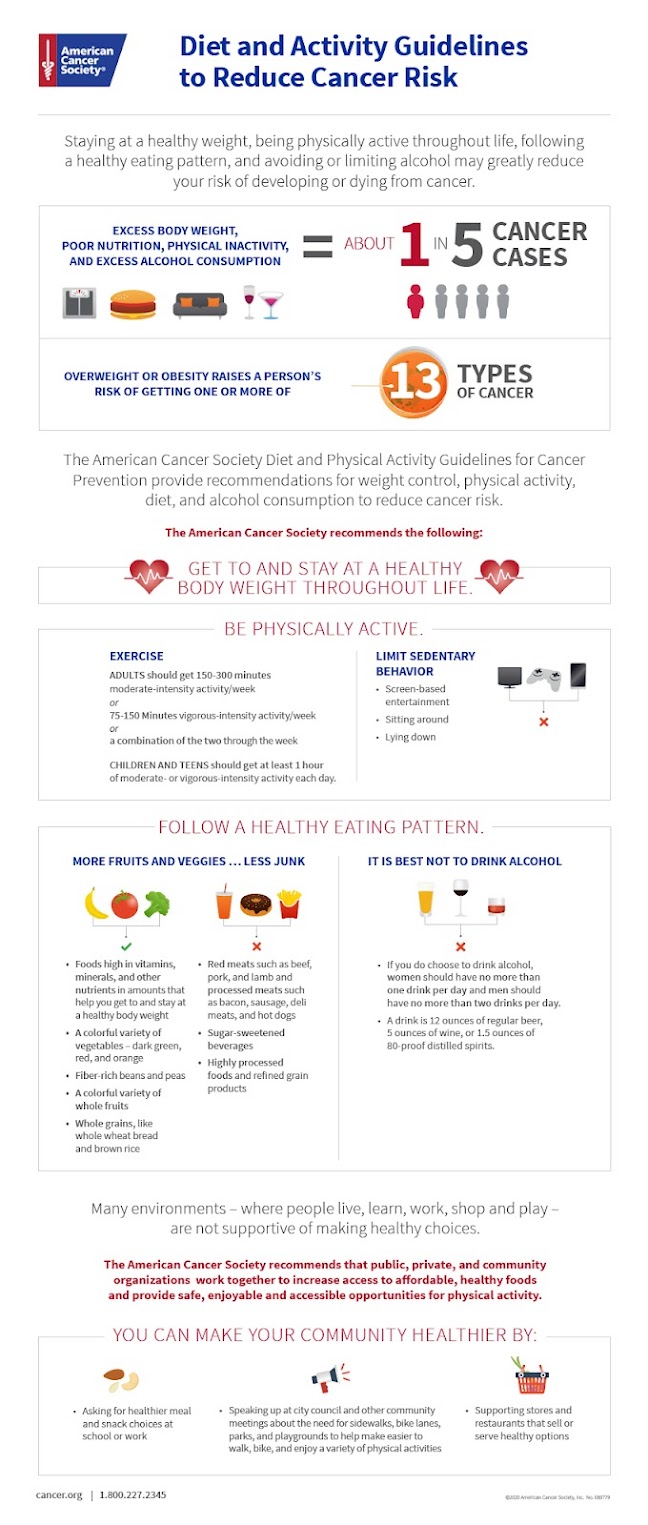
Achieve and maintain a healthy weight throughout life.
- Keep your weight within the healthy range, and avoid weight gain in adult life.
Be physically active.
- Adults: Get 150-300 minutes of moderate intensity or 75-150 minutes of vigorous intensity activity each week (or a combination of these). Getting to or exceeding the upper limit of 300 minutes is ideal.
- Children and teens: Get at least 1 hour of moderate or vigorous intensity activity each day.
- Limit sedentary behavior such as sitting, lying down, watching TV, and other forms of screen-based entertainment.
Follow a healthy eating pattern at all ages.
- A healthy eating pattern includes:
- Foods that are high in nutrients in amounts that help you get to and stay at a healthy body weight
- A variety of vegetables – dark green, red and orange, fiber-rich legumes (beans and peas), and others
- Fruits, especially whole fruits in a variety of colors
- Whole grains
- A healthy eating pattern limits or does not include:
- Red and processed meats
- Sugar-sweetened beverages
- Highly processed foods and refined grain products
It is best not to drink alcohol.
- People who do choose to drink alcohol should have no more than 1 drink per day for women or 2 drinks per day for men.
- Obesity and alcohol increase the risk of several types of cancer; these are the most important nutritional factors contributing to the total burden of cancer worldwide
- For colorectal cancer, processed meat increases risk and red meat probably increases risk; dietary fibre, dairy products, and calcium probably reduce risk
- Foods containing mutagens can cause cancer; certain types of salted fish cause nasopharyngeal cancer, and foods contaminated with aflatoxin cause liver cancer
- Fruits and vegetables are not clearly linked to cancer risk, although very low intakes might increase the risk for aerodigestive (airway and digestive tracts) and some other cancers.
Randomized controlled trials (RCTs) of dietary interventions aimed at preventing cancer, conversely, are expensive and largely impractical. Therefore, most current evidence concerning diet and cancer prevention is derived from observational epidemiologic studies, in particular prospective cohort studies, mechanistic studies of food components in laboratory animals and cell culture, and RCTs when available.
A large study (BMC Medicine 2022) that involved 79,952 US-based men found that those who ate the largest amounts of healthy plant-based foods had a 22% lower risk of bowel cancer compared with those who ate the least. The researchers found no such link for women, of whom 93,475 were included in the research. The team suggested that the link is clearer for men, who have an overall higher risk of bowel cancer.
Intermittent fasting refers to periods of restricted calorie intake or complete food avoidance. Like the Ketogenic diet, fasting triggers the use of ketones as the predominant energy source and may sensitize cancer cells to treatments and potentially slow down tumor growth. Fasting-induced metabolic changes may also favor the protection of normal tissues from therapy side effects and improve tolerance and quality of life impacts to care.
Additionally, fasting reduces insulin levels. Eating continuously can contribute to hyperinsulinemia. Elevated insulin levels are linked to an increased risk (2022) of breast, prostate, and colorectal cancers.
Cancer Fighting Foods
Do take note that we are talking about foods to prevent your risk of cancer and not about treating cancer with foods. Cancer treatments will be something that you will need to discuss with your cancer specialist.
Many foods contain beneficial compounds that could help decrease the growth of cancer. There are also several studies showing that a higher intake of certain foods could be associated with a lower risk of the disease.
We will delve into the research and look at a list of foods that may lower your risk of cancer.
1. Fruits and Berries
One large study found that participants who ate a higher amount of citrus fruits had a lower risk of developing cancers of the digestive and upper respiratory tracts (Source).
A review looking at nine studies also found that a greater intake of citrus fruits was linked to a reduced risk of pancreatic cancer (Source).
Finally, a review of 14 studies showed that a high intake, or at least three servings per week, of citrus fruit reduced the risk of stomach cancer by 28% (Source).
These studies suggest that including a few servings of citrus fruits in your diet each week may lower your risk of developing certain types of cancer.
In one human study, 25 people with colorectal cancer were treated with bilberry extract for seven days, which was found to reduce the growth of cancer cells by 7% (Source).
Another small study gave freeze-dried black raspberries to patients with oral cancer and showed that it decreased levels of certain markers associated with cancer progression (Source).
One animal study found that giving rats freeze-dried black raspberries reduced esophageal tumor incidence by up to 54% and decreased the number of tumors by up to 62% (Source).
Similarly, another animal study showed that giving rats a berry extract was found to inhibit several biomarkers of cancer (Source).
Based on these findings, including a serving or two of berries in your diet each day may help inhibit the development of cancer. Keep in mind that these are animal and observational studies looking at the effects of a concentrated dose of berry extract, and more human research is needed.
2. Turmeric (Curcumin)
3. Tomato (Lycopene)
4. Broccoli
Including broccoli with a few meals per week may come with some cancer-fighting benefits.
However, keep in mind that the available research hasn’t looked directly at how broccoli may affect cancer in humans.
Instead, it has been limited to test-tube, animal and observational studies that either investigated the effects of cruciferous vegetables, or the effects of a specific compound in broccoli. Thus, more human studies are needed.
5. Nuts
For instance, a study looked at the diets of 19,386 people and found that eating a greater amount of nuts was associated with a decreased risk of dying from cancer (Br J Nutr. 2015).
Another study followed 30,708 participants for up to 30 years and found that eating nuts regularly was associated with a decreased risk of colorectal, pancreatic and endometrial cancers (Source).
Other studies have found that specific types of nuts may be linked to a lower cancer risk. For example, Brazil nuts are high in selenium, which may help protect against lung cancer in those with a low selenium status (Trusted Source).
These results suggest that adding a serving of nuts to your diet each day may reduce your risk of developing cancer in the future.
Still, more studies in humans are needed to determine whether nuts are responsible for this association, or whether other factors are involved.
6. Olive Oil
Research has found that eating nuts may be linked to a lower risk of certain types of cancer. There are more than 1,200 search results on olive oil and cancer on PubMed.
One massive review made up of 19 studies showed that people who consumed the greatest amount of olive oil had a lower risk of developing breast cancer and cancer of the digestive system than those with the lowest intake (Source).
Another study looked at the cancer rates in 28 countries around the world and found that areas with a higher intake of olive oil had decreased rates of colorectal cancer (Source).
Swapping out other oils in your diet for olive oil is a simple way to take advantage of its health benefits. You can drizzle it over salads and cooked vegetables, or try using it in your marinades for meat, fish or poultry.
Though these studies show that there may be an association between olive oil intake and cancer, there are likely other factors involved as well. More human studies are needed to look at the direct effects of olive oil on cancer in people.
7. Carrots
For example, an analysis looked at the results of five studies and concluded that eating carrots may reduce the risk of stomach cancer by up to 26% (Source).
Another study found that a higher intake of carrots was associated with 18% lower odds of developing prostate cancer (Source).
One study analyzed the diets of 1,266 participants with and without lung cancer. It found that current smokers who did not eat carrots were three times as likely to develop lung cancer, compared to those who ate carrots more than once per week (Source).
Try incorporating carrots into your diet as a healthy snack or delicious side dish just a few times per week to increase your intake and potentially reduce your risk of cancer.
Still, remember that these studies show an association between carrot consumption and cancer, but don’t account for other factors that may play a role.
8. Beans
One study followed 1,905 people with a history of colorectal tumors, and found that those who consumed more cooked, dried beans tended to have a decreased risk of tumor recurrence (Source).
According to these results, eating a few servings of beans each week may increase your fiber intake and help lower the risk of developing cancer.
9. Soy
lower risk of breast cancer. Tofu (bean curd), is a popular food derived from soy in Asia.
A review of 35 studies (Plos One. 2014) found that soy intake could lower the risk of breast cancer for both pre- and post-menopausal women in Asian countries. However, for women in Western countries, pre- or post-menopausal, there is no evidence to suggest an association between intake of soy isoflavone and breast cancer.
Cancer and supplements
For reasons other than cancer prevention, some vitamin and/or mineral supplements may be beneficial for some people to prevent nutrient deficiency, such as in pregnant women, women of childbearing age, and people with restricted dietary intakes. Dietary supplementation may also be indicated to correct a documented clinical deficiency or insufficiency, such as supplementation with vitamin D in those with low circulating concentrations or vitamin B12 supplementation in those with vitamin B12-associated anemias.
Although a diet rich in vegetables, fruits, and other plant-based foods may reduce the risk of cancer, there is limited and inconsistent evidence that dietary supplements can reduce cancer risk (R). Whereas 2 RCTs showed reductions in cancer risk among men taking low-dose antioxidants or low-dose multiple micronutrients, evidence for women is lacking. Furthermore, evidence exists that some high-dose supplements containing nutrients such as β-carotene and vitamins A and E can increase the risk of some cancers (R). For individual nutrients, an exception may be calcium, in which supplemental calcium may reduce the risk of colorectal cancer. However, people who have excessive calcium intake (mostly from supplements) may have a higher risk of death from all cancer types combined compared with those who have a recommended level of dietary calcium. The same study also reported no overall benefit to longevity from all dietary supplements considered together. Nonetheless, more than one-half of US adults use one or more dietary supplement(s).
Many healthful compounds are found in vegetables and fruits, and it is likely that these compounds work synergistically to exert their beneficial effect. There are likely to be important, but as yet unidentified, components of whole food that are not included in dietary supplements. Some supplements are described as containing the nutritional equivalent of vegetables and fruits. However, the small amount of dried powder in such pills frequently contains only a small fraction of the levels contained in the whole foods, and there is a lack of evidence supporting a role of these products in cancer prevention. Food is the best source of vitamins, minerals, and other bioactive food components.
1. Vitamin D3, K2 and Magnesium
Vitamin D can absorb calcium and help the immune, muscle, and nervous systems function properly. There are more than 11,000 search results on vitamin D and cancer on PubMed.Several randomized trials of vitamin D intake have been carried out, but these were designed to assess bone health or other non-cancer outcomes. Although some of these trials have yielded information on cancer incidence and mortality, the results need to be confirmed by additional research because the trials were not designed to study cancer specifically.
The cancers for which the most human data are available are colorectal, breast, prostate, and pancreatic cancer. Numerous epidemiologic studies have shown that higher intake or blood levels of vitamin D are associated with a reduced risk of colorectal cancer (R). In contrast, the Women’s Health Initiative randomized trial found that healthy women who took vitamin D and calcium supplements for an average of 7 years did not have a reduced incidence of colorectal cancer (NEJM 2006). Some scientists have pointed out that the relatively low level of vitamin D supplementation (10 μg, or 400 IU, once a day), the ability of participants to take additional vitamin D on their own, and the short duration of participant follow-up in this trial might explain why no reduction in colorectal cancer risk was found.
- fatty fish
- egg yolks
- fortified milk
2. Turmeric (Curcumin)
- blocking cancer cells from multiplying
- killing colon, breast, prostate, and melanoma cancer cells
- slowing tumor growth
3. Omega-3 Fatty Acids
PubMed has indexed more than 2,900 research studies on Omega-3 and cancer. Most people use fish oil supplements to enhance the amount of omega-3’s in their diet.
Findings from a study performed in mice, research from Harvard Medical School’s Beth Israel Deaconess Medical Center in Boston demonstrated omega-3 fat could reduce tumor growth by 67% (R).
The research was presented April 4, 2022 at the annual Experimental Biology meeting in Philadelphia. The animal model showed that omega-3 fatty acids helped promote the cancer-fighting activities of immunotherapy and anti-inflammatory therapy.
Many governments recommend eating omega-3 containing fatty fish, two times per week. But that is often not enough. Ideally, people would need to eat fatty fish four times per week, while also supplementing with omega-3 fatty acids, at least 1,000 mg of pure omega-3 (DHA and EPA) per day.
However, fish oil was shown in one study on mice (2015) to possibly reduce the effectiveness of chemotherapy, and for that reason ground flax seed is a worthy alternative.
Flax seed is rich in omega-3 fatty acids, which may reduce the risk of certain cancers. When supplementing, try to avoid flaxseed oil because it lacks the nutrients of ground flax seed. Ground flax seed can be purchased online or found in many larger grocery store chains. Simply sprinkle some ground flax seed on your food and enjoy.
Make sure you buy high-quality omega-3 fatty acid supplements, meaning that the omega-3 fatty acids are pure and have not oxidized much (having low “TOTOX” value).
TOTOX value stands for total oxidation value. The omega 3 fatty acids EPA and DHA from fish oil are highly sensitive to oxidation. This means that they are rapidly affected by contact with oxygen. Oxidised fatty acids are not beneficial to our health. For this reason, a good fish oil supplement has a low TOTOX value. The maximum TOTOX value is set at 26 by the Global Organization for EPA and DHA omega-3.
The research was presented April 4, 2022 at the annual Experimental Biology meeting in Philadelphia. The animal model showed that omega-3 fatty acids helped promote the cancer-fighting activities of immunotherapy and anti-inflammatory therapy.
Make sure you buy high-quality omega-3 fatty acid supplements, meaning that the omega-3 fatty acids are pure and have not oxidized much (having low “TOTOX” value).
4. Melatonin
PubMed has indexed more than 3,300 research studies on melatonin and cancer.
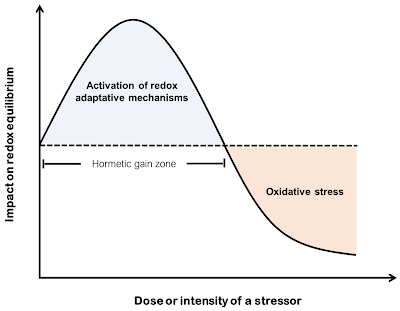
Melatonin is one of the most important antioxidant molecules. In the human body — aside from having direct antioxidant effects — it also stimulates the synthesis of glutathione and other important antioxidants like superoxide dismutase and catalase.
Many people are not aware that only 5% of your body’s melatonin — which is also a potent anticancer agent — is produced in your pineal gland. The other 95% is produced inside your mitochondria — provided you get sufficient near infrared exposure which is typically from sun on your bare skin. This is why vitamin D is more than likely a biomarker for sun exposure, which is intricately involved in melatonin production. (R)
Melatonin is known to play a fundamental role in regulating the sleep-wake rhythm; however, in the last 10 years it has been discovered that it is actually involved in many other biological mechanisms, also playing an important role in the inflammatory, metabolic and neoplastic processes. In fact, the mechanisms by which melatonin performs an anti-tumor effect are many: it has an anti-oxidant effect that protects against DNA damage, acts as a scavenger of reactive oxygen species (which undermine genomic stability), stimulates DNA repair mechanisms, improves the functioning of the mitochondrial respiratory chain, and inhibits mitochondrial mitophagy and telomerase activity (Molecules 2018).
In addition, melatonin increases the expression of the p53 protein, induces its phosphorylation, inhibiting cell proliferation, promotes apoptosis, reduces the levels of the vascular endothelial growth factor and endothelin-1, fundamental for tumor growth and metastasis formation, reduces inflammatory processes and cell migration (Molecules 2018).
Reduction of melatonin production has also been seen in some types of cancer (breast and prostate) (Mogavero 2021).
A case series of 14 advanced cancer patients (Trends in Oncology 2020), treated with high dose (1,000 mg/day) of melatonin; achieved a disease control of 54% of the patients.
The authors also concluded that:
"Moreover, this preliminary study may also suggest that high dose melatonin has no toxicity in cancer patients with poor clinical status, as well as in healthy subjects."
5. EGCG (Green Tea)
5. EGCG (Green Tea)
PubMed has indexed more than 2,000 research studies
on EGCG and cancer.
Several epidemiological studies have reported that the consumption of green
tea may decrease cancer risk. Studies have also confirmed numerous health benefits
of green tea including prevention of cancer (R, R) and cardiovascular disease, as well as
anti-inflammatory, antioxidant, antiarthritic,
antibacterial, and antiviral effects. (R, R, R, R).
Green tea also contains chemicals called polyphenols
that have antioxidant, anti-inflammatory properties
and anti-angiogenic properties, and the catechins in
green tea polyphenols show very strong anti-angiogenic
properties.
The Minnesota Green Tea Trial (MGTT. 2015) is the largest and longest
double-blind, placebo-controlled, randomized
intervention study that specifically evaluated the
effects of oral GTE (green tea extract) containing
defined quantities of EGCG on established
biomarkers of breast cancer risk.
They randomized and stratified 1075 healthy
postmenopausal women at high risk of breast
cancer according to their breast tissue density
and catechol-O-methyltransferase genotypes and
divided them into two groups: 537 placebo and
538 green tea groups. Green tea group
participants took 4 capsules that contained 843
mg EGCG, whereas the placebo group took capsules
without green tea extracts.
Researchers measured changes in percent
mammographic density, circulating endogenous sex
hormones, and proteins of the insulin-like
growth factor axis. Their results showed
that supplementation with green tea extract
could modify and reduce mammographic density
(MD) and protect against breast cancer, even
though it was only significant in younger women
(50–55 years) and had no effect in older women
(Samavat 2017), an age-dependent effect similar to
those of tamoxifen.
If you have cancer, consider drinking up to 3 cups
of green tea per day to experience the benefits.
Green tea pills are also available, but may be too
concentrated.
Some studies show health benefits in people who drink
as little as one cup per day, while other studies deem
five or more cups per day to be optimal (Source, Source).
6. Allicin (Garlic)
Garlic is a great choice when it comes to giving your body a little extra protection. To reap the benefits of garlic, you should eat one clove per day, or- antibacterial properties
- blocking and halting the activation of cancer-causing substances
- enhanced DNA repair
- a reduction in cancer cells spreading
Several clinical studies have found an association between garlic intake and a lower risk of certain types of cancer.
One study of 543,220 participants found that those who ate lots of Allium vegetables, such as garlic, onions, leeks and shallots, had a lower risk of stomach cancer than those who rarely consumed them (Source).
A study of 471 men showed that a higher intake of garlic was associated with a reduced risk of prostate cancer (Source).
Despite the promising results showing an association between garlic and a reduced risk of cancer, more human studies are needed to examine whether other factors play a role.
7. Molecular Hydrogen
More than 600 articles related to molecular hydrogen and cancer were retrieved from Cochrane, PubMed and Google Scholar, and 27 articles were included for this systematic review (2023). Based on the authors' analysis, "H2 plays a promising therapeutic role as an independent therapy as well as an adjuvant in combination therapy, resulting in an overall improvement in survivability, quality of life, blood parameters, and tumour reduction."
8. Quercetin
Quercetin is an antioxidant flavonol that's found in foods such as red grapes, green tea, elderflower and onions, to name a few. As the health benefits of the supplement become more widely known, the market has grown rapidly (R). According to market research, quercetin market was worth $261.12 million in 2020 and is expected to reach $406.58 million in 2027.2022 - A paper published in August 2022 in Nutrition Research analyzed the pro-apoptotic effect that quercetin has on aging cells. The paper reviewed preclinical and early phase data using quercetin as a senolytic agent and found the data showed it was effective in “preventing or alleviating cancer formation.”
The authors reviewed the importance of cellular aging in the development of cancer cells and the effect that quercetin may have on the suppression of cancer cell proliferation.
Cellular senescence is a dynamic and multi-step process that is associated with alterations in metabolic activity and gene expression. This can compromise tissue regeneration and contribute to aging. On the other hand, by removing senescent cells, age-related dysfunction can be attenuated and potentially extend the lifespan.
This study published in 2017 in Oncology Reports took things a step further, finding that quercetin induced cancer cell death in nine types of cancer, including prostate cancer, colon cancer, and breast caner.
In another 2017 study, researchers gave quercetin to mice with tumors. Researchers found that mice in the quercetin-treated group showed delayed tumor growth, no significant changes in daily behavior, significantly better survival ratings, and increased rates of cell death.
9. Vitamin C and B6
Sally Norton, author of “Toxic Superfoods: How Oxalate Overload Is Making You Sick — and How to Get Better,” explains:
By the third time, I became harder and harder to stab for the IV needle because now my veins were ropier and rollier and would run away from the needle. That's fibrosis ... I only had IV vitamin C maybe 10 times. But the doctor and the nurse took no notice of this side effect of the treatment — that I was becoming more fibrotic and harder to puncture ...
It's hubris to say, ‘Oh, well, it's fine. All my patients are doing great on my vitamin C IVs when you're not open to seeing the side effects. One of the studies demonstrated that just with oral supplementation, for not all that long, once they stopped the vitamin C, the level of oxalate in the urine went way up.
So, while the body's being assaulted by too much vitamin C, it's busy sequestering the oxalate that's forming and holding onto it and protecting the kidneys from devastation, from excessive oxalate load. Once you stop producing or eating too much oxalate, this holding pattern can let go, and now you see much higher oxalate levels in the blood and the urine.”
For these reasons, if you take vitamin C on a regular basis, Norton recommends limiting it to 250 mg a day. This is enough to meet your nutritional requirements and is unlikely to cause oxalic acid-related trouble. The exception would be if you are septic, in which case large doses of IV ascorbic acid can save your life.
10. Resveratrol
The efficacy, safety, and pharmacokinetics of resveratrol have been documented in over 244 clinical trials, with an additional 27 clinical trials currently ongoing (Pratap Singh 2019). Resveratrol is reported to potentially improve the therapeutic outcome in patients suffering from diabetes mellitus, obesity, colorectal cancer, breast cancer, multiple myeloma, metabolic syndrome, hypertension, Alzheimer's disease, stroke, cardiovascular diseases, kidney diseases, inflammatory diseases, and rhinopharyngitis.3.11. Gut Microbes and Probiotics
Certain gut bacteria also promote inflammation, which is an underlying factor in virtually all cancers, whereas other bacteria quell it. The presence of certain gut bacteria has even been shown to boost the patient's response to anticancer drugs. (Nature 2018)
One way in which gut bacteria improve the effectiveness of cancer treatment is by activating your immune system and allowing it to function more efficiently. Researchers have actually found that when these specific microbes are absent, certain anticancer drugs may not work at all.
Don't use tobacco
But it's not only smoking that's harmful. Chewing tobacco has been linked to cancer of the mouth, throat and pancreas.
Staying away from tobacco — or deciding to stop using it — is an important way to help prevent cancer. For help quitting tobacco, ask a health care provider about stop-smoking products and other ways of quitting.
Maintain a healthy weight and be physically active
Being at a healthy weight might lower the risk of some types of cancer. These include cancer of the breast, prostate, lung, colon and kidney.Physical activity counts too. Besides helping control weight, physical activity on its own might lower the risk of breast cancer and colon cancer.
Doing any amount of physical activity benefits health. But for the most benefit, strive for at least 150 minutes a week of moderate aerobic activity or 75 minutes a week of hard aerobic activity.
You can combine moderate and hard activity. As a general goal, include at least 30 minutes of physical activity in your daily routine. More is better.
Avoid risky behaviors
Another effective cancer prevention tactic is to avoid risky behaviors that can lead to infections that, in turn, might increase the risk of cancer. For example:
-
Practice safe sex. Limit the number of sexual partners and use a condom. The greater the number of sexual partners in a lifetime, the greater the chances of getting a sexually transmitted infection, such as HIV or HPV.
People who have HIV or AIDS have a higher risk of cancer of the anus, liver and lung. HPV is most often associated with cervical cancer, but it might also increase the risk of cancer of the anus, penis, throat, vulva and vagina.
- Don't share needles. Injecting drugs with shared needles can lead to HIV, as well as hepatitis B and hepatitis C — which can increase the risk of liver cancer. If you're concerned about drug misuse or addiction, seek professional help.
Protect yourself from the sun
Skin cancer is one of the most common kinds of cancer and one of the most preventable. Try these tips:
- Avoid midday sun. Stay out of the sun between 10 a.m. and 4 p.m. when the sun's rays are strongest.
- Stay in the shade. When outdoors, stay in the shade as much as possible. Sunglasses and a broad-brimmed hat help too.
- Cover your skin. Wear clothing that covers as much skin as possible. Wear a head cover and sunglasses. Wear bright or dark colors. They reflect more of the sun's harmful rays than do pastels or bleached cotton.
- Don't skimp on sunscreen. Use a broad-spectrum sunscreen with an SPF of at least 30, even on cloudy days. Apply a lot of sunscreen. Apply again every two hours, or more often after swimming or sweating.
- Don't use tanning beds or sunlamps. These can do as much harm as sunlight.
Sleep, Stress and Desk Job
The American Cancer Society has also found a link between long periods of inactivity and cancer. The group says that people who spend "prolonged leisure time sitting" — defined as more than 6 hours per day — have a 19% higher rate of death compared to people who sit an average of 3 hours per day. That number includes all causes of death, but it doesn't necessarily mean that sitting directly causes cancer or other diseases, since sick people are also likely to move around less.
.png)
.png)

.png)

.jpg)



Comments