Guide to Anti Aging and Longevity 101: The Science (2024 Edition)
The process of human aging is a complex and multifactorial process. NAD, stem cells, nitric oxide, glutathione, vitamin B12, CoQ10, glycine, taurine and testosterone decline as we age. Vitamin and mineral deficiencies are also common in older individuals.
Methodology: The selection or short-listing of the topics below is based on the available scientific evidence retrieved from scientific database such as PubMed and scientific search engine such as Google Scholar. The article will also be updated as and when there is a newly discovered major research publication related to anti-aging and longevity.
- What is Aging?
- Biological Age vs Chronological Age
- Causes of Aging
- What is Cell Senescence?
- What is Epigenetics?
- Diet and Lifestyle for Anti Aging
- Healthy Lifestyle
- Mediterranean Diet
- Exercise and Resistance Training
- Stress Management
- Caloric Restriction, Intermittent fasting (Time Restricted Eating) and Fasting
- Avoiding Linoleic Acid (Omega-6 Fatty Acids) and Vegetable Oil
- Avoiding Ultra-Processed Foods
- Sleep
- Social Support
- Best Scientifically Proven Anti Aging Supplements
- Stem Cell Therapy for Anti-Aging
- Hormone Replacement Therapy
- Peptide Therapy for Anti Aging
- Exosomes for Anti Aging
- What is mTOR (Mammalian Target of Rapamycin)?
- Conclusion and Key Takeaways
What is Aging?
 |
| Longevity Medicine will become the New Primary Care |
Biological Age vs Chronological Age
But maybe your doctor says you have the physical conditioning of a 21-year-old. This would be considered your biological age, regardless of how many years ago you were born.
Your chronological age will always be an easy-to-determine number, while your biological age depends on a number of variables that can change on a continuing basis.
What is chronological aging?
It’s also a primary risk factor for chronic diseases, mortality, and any impairments to bodily functions, such as hearing and memory.
What is biological aging?
Also known as physiological or functional age, biological age differs from chronological age because it takes into consideration a number of factors other than just the day you were born.
The actual number comes down to different biological and physiological development factors. Some of these include:
- chronological age
- genetics (for example, how quickly your body’s antioxidant defenses kick in)
- lifestyle
- nutrition
- diseases and other conditions
While chronological age is a factor, you may not end up having the same biological age as your chronological age. For example, if you’re a 28-year-old male who doesn’t exercise, only eats high-fat foods, and has smoked five packs of cigarettes per day for the last 10 years, it’s likely you would have a biological age of greater than 28 years.
 |
| Image credit: Longevity.technology |
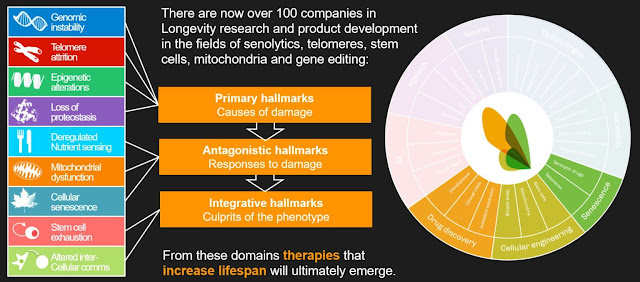
Causes of Aging
- genomic instability,
- telomere attrition,
- epigenetic alterations,
- loss of proteostasis,
- deregulated nutrient-sensing,
- mitochondrial dysfunction,
- cellular senescence,
- stem cell exhaustion,
- altered intercellular communication,
- disabled macroautophagy, (new)
- chronic inflammation, and (new)
- dysbiosis. (new)
 |
| Source: Cell 2023 |
- Meta-analysis and Randomised controlled trials (RCTs)
- Large clinical trials (phase 3)
- Small clinical trials (phase 2) and Case studies
- Mouse results and animal studies
- In Vitro, cell culture, commentary, review, expert opinions and anecdotal evidence
 |
| Credit: ACS Chem. Neurosci. 2024 |
 |
| Credit: ACS Chem. Neurosci. 2024 |
 |
| Connecting the dots between Antiaging nutrients and drugs and (A) hallmarks of aging, and (B) antiaging strategies. Credit: ACS Chem. Neurosci. 2024 |
What is Cell Senescence?
- Interfere with organ function (heart, brain, liver, kidney, skin…)
- Create age related diseases (cardiovascular, kidney, diabetes…)
- Shorten healthy lifespan (decrease function and create disease)
- Accelerate degeneration (damage causes breakdown)
- Damage organs (colon, blood vessels, nervous system…)
- Triggers inflammation causing problems (high blood pressure, elevated cholesterol, elevated blood sugar….)
What is Epigenetics?
Diet and Lifestyle for Anti Aging
That's according to research presented in July 2023 at the American Society for Nutrition’s annual conference in Boston. (SciTechDaily)
@dr.kevin.reese Everything has a root cause…
♬ original sound - Dr. Kevin Reese, PhD, PAS, DS
1. Diet and Healthy Lifestyle studies
In this study (Sakaniva 2022), 45,021 people were studied from 1988 to 1990 and the subjects continued to be monitored until 2009. Each healthy lifestyle factor like diet, exercise, smoking, sleep, and BMI (body mass index) was given a point.2. Diet
@lewis Biochemist Jessie Inchauspé aka @glucosegoddess_ shares incredible hacks in this episode to minimize glucose spikes without cutting sugar out of your diet - have you listened yet? #sugar #sciencetok #aging #reverseaging #glucose #glucosegoddess #jessieinchauspe #jessieinchauspé #biochemistry #nutrition #nutritiontips #healing #healingjourney #wellness #wellnesstips #healthandwellness #healthandwellnesstips #food #glycation #ageinreverse #nutritionhacks #biohack #biohackingsecrets ♬ Adventurer - Lux-Inspira
3. Avoiding Linoleic Acid, Vegetable Oil and Ultra-Processed Foods
Over the last century, thanks to fatally flawed research suggesting saturated animal fat caused heart disease, the LA in the human diet has dramatically increased, from about 2 to 3 grams a day 150 years ago, to 30 or 40 grams a day.
On a side note, do not confuse LA with conjugated linoleic acid (CLA). While most think CLA and LA are interchangeable, they're not. CLA has many potent health benefits and will not cause the problems that LA does.
Like other nutrition experts, study author Nilson agreed that a healthy, balanced diet should be based on fresh and minimally processed foods, when possible, in addition to avoiding ultra-processed foods.
“The continuity of the current trends with gradual increases in ultra-processed food consumption will increase premature deaths,” Nilson said, adding that his research highlights a need for a shift in policy around ultra-processed foods.
4. Avoiding Smoking
“Smoking is one of the strongest risk-factors for every chronic disease, including heart disease and cancer,” says Susan Lakoski, M.D., associate professor of cancer prevention at MD Anderson Cancer Center.Smoking and secondhand smoke introduce harmful toxins to the body. There’s no such thing as a healthy smoker - especially when it comes to cancer prevention.
“The biggest myth I hear is that if someone exercises they can offset the negative effects from smoking, but that’s absolutely not the case,” says Susan Lakoski, M.D.
But it's not only smoking that's harmful. Chewing tobacco has been linked to cancer of the mouth, throat and pancreas.
Staying away from tobacco — or deciding to stop using it — is an important way to help prevent cancer. For help quitting tobacco, ask a health care provider about stop-smoking products and other ways of quitting.
5. Avoiding Alcohol
6. Sleep
This is one of the most under-rated anti-aging strategies. Research has demonstrated sleep is a crucial component of a healthy lifestyle.
In a 2023 study (The Lancet), scientists looked at how the relationship between sleep and exercise might impact cognitive decline. Researchers from University College London examined the association between physical activity and sleep duration in 8,958 participants over 10 years. The data were collected from the English Longitudinal Study of Aging, during which participants were interviewed every two years.
The researchers evaluated episodic memory using recall tasks and verbal fluency using animal naming tasks. They found that participants with lower levels of physical activity and suboptimal sleep had worse performance on the cognitive tests and those who slept the least exhibited faster cognitive decline. Interestingly, the participants who had higher levels of physical activity and shorter sleep times also had faster rates of cognitive decline.
Those who had higher levels of physical activity and slept an optimal number of hours had the slowest cognitive decline. Overall, the data suggested that higher-intensity physical activity was not enough to mitigate the rapid cognitive decline that is associated with insufficient sleep.
Lack of quality sleep can also weaken immune function and increase susceptibility to respiratory infections, including the common cold, and chronic lack of sleep may be associated with an increased risk of death (Prather 2015; Ibarra-Coronado 2015; Wilder-Smith 2013; Aldabal 2011).
Sleep deprivation is associated with elevated cortisol levels, as well as higher daytime levels of inflammatory cytokines including IL-1, IL-6, and tumor necrosis factor-alpha (Aldabal 2011; Hirotsu 2015). A study in individuals aged 61‒86 found even a single night of partial sleep deprivation induced patterns of gene activation associated with biological aging (Carroll 2016).
7. Stress Management
A big component of the longevity equation is the management of stress.
A June 2022 study supports what immunologists have long suspected: A key stressor to our immune system as we age may be stress itself.
“Immune aging may help explain why older people tend to benefit less from vaccines and why they have more serious complications associated with infections like COVID-19,” Erik Klopack, Ph.D., a lead author of the study and a postdoctoral scholar at the Leonard Davis School of Gerontology at the University of Southern California. “Our study suggests that social stress may accelerate immune aging,” he said.
8. Exercise and Resistance Training
Another important factors in slowing sarcopenia is diet. As we age our appetite declines, so as we eat less we naturally reduce the amount of protein that we consume. To slow sarcopenia we need to keep our protein intake high, and as we are eating less this means that a higher proportion of the food we eat needs to be protein. It is also important to spread this protein out through the day over three or meals as this produces more muscle protein synthesis when compared to one or two high protein meals.
It is also important to get your vitamin D levels checked as you age since deficiency is common due to reduced sun exposure. As well as weakening our bones, low vitamin D results in weaker muscles and accelerated sarcopenia. A low vitamin D level can be easily rectified with supplementation. When was the last time you had your vitamin D level checked?
Being aware that sarcopaenia affects us all is the first step in combating its effects. The earlier you commence resistance exercise, the greater the benefits, but it is never too late to start. If you are new to resistance exercise or intimidated by the gym environment, talk to your local gym about some personal training to help you learn.
9. Social Support
Okinawa in Japan, Sardinia in Italy, Roseto in Pennsylvania, Loma Linda in California, Icaria in Greece and Nicoya in Costa Rica are some of the places with the highest proportions of people who live to be 100 years old.
All these places have the same thing in common. What is it?
10. Intermittent fasting, time restricted eating (TRE) and Calorie Restriction
Intermittent fasting is currently one of the most popular nutrition programs around. Unlike diets that tell you what to eat, intermittent fasting focuses on when to eat.
Limiting the hours you eat each day may help you consume fewer calories. It may also provide health benefits, including weight loss and improved heart health and blood sugar levels.
There are several forms of intermittent fasting, including a common form called time-restricted eating.
Research overwhelmingly supports the notion that ditching the three square meals a day approach in favor of time-restricted feeding — can do wonders for your health. Contrary to modern belief, your body isn't designed to be fed throughout the day, and the near-continuous grazing that most engage in can have serious health consequences.
Time-restricted eating is just what it sounds like. It's a form of intermittent fasting where you eat all of your meals for the day within a restricted window of time, ranging from two to eight hours. That means you're avoiding food (fasting) for 16 to 22 consecutive hours. Eating within a four- to six-hour window is likely close to metabolic ideal for most. As noted in the paper "A Time to Fast," published in the November 2018 issue of Science:
"Adjustment of meal size and frequency have emerged as powerful tools to ameliorate and postpone the onset of disease and delay aging, whereas periods of fasting, with or without energy intake, can have profound health benefits.
The underlying physiological processes involve periodic shifts of metabolic fuel sources, promotion of repair mechanisms, and the optimization of energy utilization for cellular and organismal health …
In general, both prolonged reduction in daily caloric intake and periodic fasting cycles have the power to delay the onset of disease and increase longevity."
Fasting, or reducing your calorie intake is also an excellent method for indirectly boosting the body’s NAD levels. Fasting has been shown to increase the levels of NAD+ and surtuins; the proteins which have been found to slow the aging process.
While fasting is effective in increasing NAD+ levels, drastic reduction in calorie intake or fasting can have a counterproductive effect. There is also some speculation that intermittent fasting or adopting a low carb-ketogenic diet may also provide similar positive results.
Research also suggests that caloric restriction and fasting might be helpful to give your existing so-called endogenous stem cells a boost.
Fasting may also help reduce obesity-associated cancers. “There’s a lot of obesity-associated cancers,” said Dr. Jason Fung, a nephrologist and fasting expert. “There’s about 13 cancers that are well accepted that they are associated with obesity; fasting might help decrease that.”
Fasting can potentially starve cancer cells. When fasting, the body uses fats and produces ketones for energy. Cancer cells rely heavily on glucose, making them less efficient at using ketones.
Additionally, fasting reduces insulin levels. Elevated insulin levels are linked to an increased risk of breast, prostate, and colorectal cancers.
Caloric Restriction
The goal of caloric restriction is to reduce total caloric intake while maintaining optimal nutrition. This may be best accomplished by eating a diet primarily composed of low-calorie, nutrient-dense foods such as vegetables, fruits, legumes, nuts and seeds, and whole grains; limiting intake of animal products; and avoiding calorie-dense, nutrient-poor foods (Rizza 2014). Caloric restriction in animals has been shown to prolong lifespan and delay aging, and to confer a more youthful profile of T cells (Ahmed 2009; Fernandes 1997; Michan 2014).
Limiting the hours you eat each day may help you consume fewer calories. It may also provide health benefits, including weight loss and improved heart health and blood sugar levels.
There are several forms of intermittent fasting, including a common form called time-restricted eating.
"Adjustment of meal size and frequency have emerged as powerful tools to ameliorate and postpone the onset of disease and delay aging, whereas periods of fasting, with or without energy intake, can have profound health benefits.
The underlying physiological processes involve periodic shifts of metabolic fuel sources, promotion of repair mechanisms, and the optimization of energy utilization for cellular and organismal health …
In general, both prolonged reduction in daily caloric intake and periodic fasting cycles have the power to delay the onset of disease and increase longevity."
Fasting can potentially starve cancer cells. When fasting, the body uses fats and produces ketones for energy. Cancer cells rely heavily on glucose, making them less efficient at using ketones.
Additionally, fasting reduces insulin levels. Elevated insulin levels are linked to an increased risk of breast, prostate, and colorectal cancers.
Best Anti-Aging Supplements
There are a lot of options out there, and we know it can be overwhelming.
What are the best anti-aging supplements? Are they the Elixir of Youth?
Although many main-stream media channels may state that there is no scientific evidence to support the effectiveness of any specific supplements, it's definitely not true. There are countless anti-aging supplements that are supported by overwhelming scientific evidence out there. However, most of them are based on outdated science, not supported by well-conducted scientific studies or not scientifically proven, focus on aging process that are less relevant, contain doses that are too low, and are not verified in humans.
It's crucial to understand the limitations of conventional medicine when exploring the subject of anti-aging supplements. Most doctors may not have much to offer in the anti-aging space, as the focus of conventional medicine involves treating diseases reactively with drugs and surgery. However, recent scientific studies have proven the effectiveness of many anti-aging supplements, but it's essential to choose the ones that are scientifically proven, based on up-to-date science, and verified in humans.
To delve into the latest research on anti-aging supplements and gero-protectors, check out "Best Anti Aging Supplements" (2024 Edition).
To delve into the latest research on anti-aging supplements and gero-protectors, check out "Best Anti Aging Supplements" (2024 Edition).
Most officially recommended daily doses are too low
You should know that the official recommended dietary allowances of vitamins and minerals, as defined by government agencies, are often just the bare minimum you need to take in to not become sick. They do not tell you what are the best amounts for a long, optimal, healthy life.
Most of these official recommendations are also based on old studies in which volunteers were deprived of a specific vitamin or mineral. Scientists then waited a while until people became sick, and then determined the minimum dose you would need to prevent this.
So these recommended daily intakes are what you need to take on a daily basis in order not to become sick after a number of months (the duration of the study). They do not tell you the ideal amounts you need to stay healthy and slow down aging for decades to come.
Take for example vitamin B12. The recommended dietary allowance is around 2.4 mcg in many countries. But that’s in fact the “minimum” amount you need to not become sick after a few months or years, getting serious complications, like anemia, fatigue or cognitive problems. This doesn’t mean this is the optimal amount for a long, healthy life.
For example, we see in studies that you need at least 20 mcg of vitamin B12 to optimally protect the DNA against DNA strand breaks – more than 8 times greater than the recommendation!
Also, many people do not take up vitamin B12 well, especially as we get older. For example, atrophic gastritis affects at least 10 to 30 percent of people older than 60, leading to malabsorption of vitamin B12. So, they would need far more vitamin B12 than advised by governments.
In fact, The Linus Pauling Institute at Oregon State University recommends that all people older than 50 take at least 100 to 400 ug/day of supplemental vitamin B12 (R). That’s considerably more than the 2.4 mcg many governments advise.
It’s interesting to see that many foods rich in vitamin B12 (clams, mussels, crab, and fish like mackerel and salmon) are water-borne foods. Scientists speculate that people evolved for tens of thousands of years living close to shorelines and rivers and lakes and consumed high amounts of sea food and thus vitamin B12 (R), probably reaching daily intake levels far more than a meagre 2.4 mcg per day.
These are just a few examples demonstrating that yes, we need to take supplements for optimal aging. And this for the rest of our lives, and even more when we are older and suffer from age-related malabsorption issues and changes that hinder us to properly use these important vitamins and minerals.
Most of these official recommendations are also based on old studies in which volunteers were deprived of a specific vitamin or mineral. Scientists then waited a while until people became sick, and then determined the minimum dose you would need to prevent this.
So these recommended daily intakes are what you need to take on a daily basis in order not to become sick after a number of months (the duration of the study). They do not tell you the ideal amounts you need to stay healthy and slow down aging for decades to come.
Take for example vitamin B12. The recommended dietary allowance is around 2.4 mcg in many countries. But that’s in fact the “minimum” amount you need to not become sick after a few months or years, getting serious complications, like anemia, fatigue or cognitive problems. This doesn’t mean this is the optimal amount for a long, healthy life.
For example, we see in studies that you need at least 20 mcg of vitamin B12 to optimally protect the DNA against DNA strand breaks – more than 8 times greater than the recommendation!
Also, many people do not take up vitamin B12 well, especially as we get older. For example, atrophic gastritis affects at least 10 to 30 percent of people older than 60, leading to malabsorption of vitamin B12. So, they would need far more vitamin B12 than advised by governments.
In fact, The Linus Pauling Institute at Oregon State University recommends that all people older than 50 take at least 100 to 400 ug/day of supplemental vitamin B12 (R). That’s considerably more than the 2.4 mcg many governments advise.
It’s interesting to see that many foods rich in vitamin B12 (clams, mussels, crab, and fish like mackerel and salmon) are water-borne foods. Scientists speculate that people evolved for tens of thousands of years living close to shorelines and rivers and lakes and consumed high amounts of sea food and thus vitamin B12 (R), probably reaching daily intake levels far more than a meagre 2.4 mcg per day.
These are just a few examples demonstrating that yes, we need to take supplements for optimal aging. And this for the rest of our lives, and even more when we are older and suffer from age-related malabsorption issues and changes that hinder us to properly use these important vitamins and minerals.
Stem Cell Therapy for Anti-Aging
Despite the fact that there are many published studies on stem cell therapy for anti-aging, major media has been slow to report the findings.
The Vinmec Research Institute of Stem Cell and Gene Technology are exploring the use of MSC for male sexual dysfunction in a phase I/II clinical trial (NCT05345418). They are currently recruiting male subjects aged 50–70 years old with sexual functional deficiency. Treatment groups will receive two iv doses of 1.5 million cells/kg body weight spaced out by 3 months. Various biomarkers, testosterone levels, and sexual life quality information will be measured. The First Affiliated Hospital with Nanjing Medical University has an upcoming phase I clinical trial (NCT04706312) researching the use of amniotic mesenchymal stem cells (AMSCs) for the treatment of infertility is people with diminished ovarian response. Subjects will receive an iv injection of AMSCs and measurements recorded for ovarian function and in vitro fertilization such as stimulated follicles, number of oocyte retrieval, fertilization rate, etc. (ACS Chem. Neurosci. 2024)
Hormone Replacement Therapy
Hormone replacement therapy (HRT) for women has been a topic of much debate in recent decades. This is due largely to the fact that the Women’s Health Initiative (WHI) study in 2002 was halted prematurely because of a reported increase in the instance of breast cancer in women participating in the hormone replacement arm of the study. Thereafter, thousands of women were taken off or stopped taking HRT unnecessarily, despite the fact that many studies have debunked the WHI conclusions.
HRT & Breast Cancer: What’s the Connection?
One of the major flaws of the WHI was the confusion and fear it spread by projecting its results to all women receiving HRT. In the original study, more women who took estrogen plus progestin (E+P) developed breast cancer than those taking placebos.
Further research published in a 2013 article in The Journal of Clinical Endocrinology and Metabolism shows that breast cancer rates were actually found to decrease significantly with estrogen alone. Moreover, the article goes on to say that even though there isn’t a significant increase with E+P used together versus estrogen alone, for illustrative purposes, any increased risk of breast cancer associated with E+P originally publicized with the WHI trial is less than the risk conferred by obesity, being a flight attendant, and many other common exposures.
Another noteworthy difference which can play a role in breast cancer risk is the use of synthetic progestins versus bioidentical progesterone. Synthetic progestins, which were used in the WHI, are hormones which are synthetically produced, and thus different in structure from bioidentical progesterone. Bioidentical progesterone, while produced from a plant source, is structurally and chemically identical to the progesterone produced by the ovaries. Synthetic progestins mimic some effects of the natural hormone, but react differently with progesterone receptors within the body and are felt to be responsible for the increase in breast cancer seen in WHI. On the other hand, bioidentical progesterone does not increase, and may actually reduce the risk of breast cancer.
Can HRT Help Prevent Cardiovascular Disease in Women?
Cardiovascular disease is responsible for 1 in every 4 deaths in the U.S. It’s the leading cause of death in both men and women, and leads to more than 600,000 deaths across the country annually (CDC). It’s therefore critical that as the risk for cardiovascular disease increases with age, individuals find ways to optimize heart health.
HRT may not be prescribed for women primarily as a means for improving cardiovascular health, but this is indeed a powerful byproduct of the treatment. According to research published in the BMJ, women receiving HRT early after experiencing menopause had a significantly reduced rate of heart failure, myocardial infarction, and mortality overall. At the start of treatment, women on average were aged 50 and had been postmenopausal for seven months. Roughly half as many women using HRT experienced cardiovascular events compared to those in the control group. Additionally, these results did not correlate with an increased risk in any cancer [BMJ 2012].
Moreover, evidence shows that there is a clear benefit in using estrogen alone, with coronary calcium scores significantly reduced. This measures the buildup of calcium and other substances which can narrow or close the arteries, leading to cardiovascular issues. In particular, women under 60 who receive hormone therapy have a statistically significant reduction in coronary disease (Lobo 2013).
These aren’t the only positive outcomes of HRT, however. Hormone therapy has been commonly used as an osteoporosis preventative, which brings us to our next segment.
Testosterone injections are most often given by your doctor. The injection site is typically in the gluteal muscles in the buttocks.
TRT is an acronym for testosterone replacement therapy, sometimes called androgen replacement therapy. It’s primarily used to treat low testosterone (T) levels, which can occur with age or as a result of a medical condition.
But it’s becoming increasingly popular for non-medical uses, including:
- enhancing sexual performance
- achieving higher energy levels
- building muscle mass for bodybuilding
This is all part of a completely natural process that starts in your late 20s or early 30s.
This gradual decrease in Testosterone often doesn’t cause any noticeable symptoms. But a significant drop in T levels may cause:
- low sex drive
- fewer spontaneous erections
- erectile dysfunction
- lowered sperm count or volume
- trouble sleeping
- unusual loss of muscle and bone density
- unexplained weight gain
DHEA plays a critical role by serving as a counterweight to cortisol. Cortisol is an adrenal hormone with immunosuppressive properties, while DHEA may have direct immunostimulating properties: in a laboratory study of white blood cells from donors who were at least 65 years old, DHEA treatment reversed the age-related reduction of specific receptors on immune cells and increased immune cell responsiveness (Corsini 2005). Although DHEA levels decline dramatically with age, cortisol levels remain relatively constant, leading to an imbalance of these two hormones that is believed to contribute to immune senescence (Buford 2008; Buoso 2011).
Exosome Therapy for Anti Aging
- Manage degenerative conditions
- Repair degenerated and damaged tissue
- Powerful anti-inflammatory effects
- Promising anti-aging capabilities
- Improve pain control
- Decrease brain inflammation
Peptide Therapy for Anti Aging
- BPC-157
- CJC-1295 with Ipamorelin
- Epithalon (Epitalon)
- Alleviate aches and pain
- Promoting tissue healing
- Heal and unhealthy gut
- Maintain a newly healed healthy gut
- Increase in lean muscle mass
- Decrease in body fat percentage
- Increased collagen, elastin, and fibrin production for younger skin
- Increase in restful sleep
- Increase in energy levels
- Improved cardiovascular function
- Stronger immunity
- Decreased joint and muscle pain
- Enhanced healing after injury
- Increases telomerase
- Improving telomere health
- Cellular regeneration
- Improves autophagy
- Expands gene expression
What is mTOR?
- Significant benefits in cardiovascular function with reversal or attenuation of age-related changes in the heart
- Beneficial behavioral, skeletal and motor changes compared with mice fed a control diet
- Reduced indicators of inflammatory, metabolic, and hypertrophic expression of cardiac tissues
- A decrease in cancer incidence
- Improvement of cardiac function (heart function)
- Improvement in bone marrow function (immune system)
- Metabolizes cellular fat stores (weight and body composition)
- Increases lifespan by inhibiting mTOR (slows down rate of aging)
- A highly-optimized diet
- Individualized power supplements
- A healthy sleep routine
- Stress management techniques
Conclusion and Key Takeaways
The best way to promote longevity and overall health is to engage in healthy practices like consuming a nutritious diet, engaging in regular exercise, improving your sleep and reducing stress.While some research suggests potential benefits from supplements, hormone therapy, or even stem cells in slowing aging, these shouldn't replace core healthy practices. A well-rounded approach is key for optimal well-being.
Focus on Fundamentals:
- Nutritious Diet: Prioritize a balanced diet rich in fruits, vegetables, and whole grains.
- Regular Exercise: Aim for consistent physical activity, incorporating different types like cardio and strength training.
- Quality Sleep: Get enough restful sleep for optimal body and brain function.
- Stress Management: Find healthy ways to manage stress, such as meditation or spending time in nature.
Supplements: A Supportive Role
Remember, supplements are not magic bullets. They should complement, not replace, a healthy lifestyle. Consult your doctor before starting any new supplement program to ensure safety and suitability for your individual needs.
Multi-Faceted Aging Solutions
Aging is a complex process with various contributing factors. Ideally, an anti-aging supplement should address these factors synergistically, meaning the components work together for a stronger effect.
- Epigenetics: Look for substances supporting a healthy epigenome, like alpha-ketoglutarate (AKG) and NMN.
- Mitochondrial Health: Consider ingredients like AKG, fisetin, and malate to support healthy mitochondrial function.
A Holistic Approach
Remember, there's no one-size-fits-all solution to aging. A well-rounded approach that combines a healthy lifestyle with potential benefits from evidence-based supplements might be the best strategy.
Reliable Research:
Always prioritize credible sources for information. Look for research published in peer-reviewed journals, searchable through platforms like PubMed or Google Scholar.







.png)
Comments